|
Many times I've been at births where the nurse or midwife or OB says to my client "Did you take a birth class?" only to follow it up with "Did you learn how to push?" I always find this question so interesting because in an unmedicated birth, pushing has the potential to be an involuntary response. The mass of muscle that has collected at the top of the uterus has been building up, harnessing its strength and power for the very moment when the baby has angled its head just right to fit through the narrow space at the mid pelvis and then dropped a bit lower to begin extending its head under the pubic bones. The uterus has been waiting for this!
But there is this myth out there that people have to be trained in how to push their babies out. And yes, many times some guidance can be very helpful. There are a few times when Valsalva pushing may be a useful option - if a medicated labor decreases the ability to feel the pressure of the baby descending, if spontaneous pushing in a medicated or unmedicated birth does not lead to progress (after significant time and changing of positions, not just one or two contractions), or if a concern about the baby's well being is requiring the second stage to move along faster (more on this later). However, if all is going well and the laboring person has enough sensation to feel what is happening in their body, there are some clear reasons why someone may be better off pushing on their own. Directed pushes - when a deep inhale is taken and while holding the breath, the laboring person pushes for ten seconds, then repeats this again for a total of three "pushes" during the length of one contraction - are extremely strong which can be helpful for expediting the pushing phase when there is a great concern about the baby's well being. Research is mixed on whether or not it decreases the length of the second stage of labor. These pushes can damage the ligaments of the perineal area (see our previous post about keeping the perineum intact) which can complicate the healing process postpartum and potentially lead to pelvic floor dysfunction such as prolapse and incontinence and decreased bladder capacity. While this mode of pushing is usually stalled, as the baby's head begins to crown, in an effort to protect the superficial perineal muscles (and therefore prevent or minimize "tearing") , the damage to the underlying structures is already done at this point. This directed pushing - also known as Valsalva pushing - can also lead to extreme headaches, burst blood vessels in the eyes, decreased blood flow to the baby, and a subsequent need for an oxygen mask for the laboring person. If a baby was in distress during the pushing phase of the second stage, some providers encourage Valsalva pushing to expedite the labor process. However, because this decreases blood flow to the placenta, it may actually further encourage distress in the baby. Research advises giving the baby a rest from pushing, skipping pushing during a few contractions, and possibly continuing then to push only with every other or every three contractions. Spontaneous pushing - which is often more of an exhalation followed by a push that may last five to six seconds, possibly done twice during the length of one contraction - has far less intense pressure placed immediately upon the perineal structures. This allows the muscles to relax with the force of pressure rather than respond by tightening. In addition, the pressure is more directly focused on the vagina and anterior portion of the perineal area which may lessen the risk of tearing. It is also noted that spontaneous pushing may lead to better APGAR scores for newborns as well as less maternal fatigue (which has the potential to affect maternal/fetal bonding and breastfeeding). In conclusion, the research clearly shows benefits to spontaneous pushing yet it appears that hospital staff is not always on board. This means that a discussion of pushing techniques is an important discussion to have with one's provider prior to reaching the second stage of labor. Although some may choose to add a desire for spontaneous pushing into a written birth plan, nothing can replace the verbal reminder to a provider that the research shows spontaneous pushing is the way to go in a low risk scenario. Sources Cited: Calais-Germain, Blandine. The Female Pelvis: Anatomy & Exercises. Eastland Press, 2003. Gulay, Yildirim, Nezihe Kizilkaya Beji. "Effects of Pushing Techniques in Birth on Mother and Fetus: A Randomized Study. Birth 2008; 35;1: 25-30. Hamilton, Cathy. "Using the Valsalva technique during the second stage of labor." British Journal of Midwifery 2014. Haseeb Yasmeen A, Alkunaizi Anwar N, Al Turki Haifa, Aljama Fathia, Sobhy Soheir I. "The impact of valsalva's versus spontaneous pushing techniques during second stage of labor on postpartum maternal fatigue and neonatal outcome." Saudi Journal of Medicine and Medical Sciences 2014; 2:2:101-105. Prins M, Boxem J, Lucas C, Hutton E. "Effect of spontaneous pushing versus Valsalva pushing in the second stage of labour on mother and fetus: a systematic review of randomised trials." BJOG 2011;118:662–670. SImpson, Kathleen Rice. "When and How to Push: Providing the Most Current Information About Second-Stage Labor to Women During Childbirth Education." The Journal of Perinatal Education 2006; 15(4): 6-9.
0 Comments
During the dog days of summer, it can get pretty hot (and sweaty) when feeding baby. So how do you keep yourself and baby cool? A few of the BRC Board members wanted to share some tips to beat the heat while feeding baby. And of course, all of these are BRC Lactation Consultant approved too.
Babies don’t need water -- breastmilk is just fine. Babies don’t need additional water when it’s hot outside. According to WHO, and our in-house experts agree, breastmilk is more than 80% water, especially the first milk that comes with each feed. Therefore, anytime you feel baby is thirsty feel free to nurse. No water needed. On the subject of water… hydration for [the breastfeeding person] is important. Of course, we all know on the hottest of days it’s important to stay well hydrated. But it’s a critical aspect of milk production too so keep drinking that water. Our IBCLCs recommend drinking to thirst. Parents tend to be more thirsty when nursing therefore always have a water bottle close by. Pack a light blanket. It’s great to get outside in the summertime, so having a lightweight nursing cover is important if you chose to cover up when you nurse in public. Pick something like muslin, a light cotton weave, which are easy to find at Target or on Amazon. Dress to stay cool and comfortable. There are a lot of clothing options for a breastfeeding parent to stay cool in the summer and accessible to baby. Things like nursing bra tanks and dresses that button up the front usually work best. For more recommendations, check out “What to Wear When Breastfeeding in Summer” by Morgan Manages Mommyhood -- there are a lot of great tips and recommendations. Plan ahead for high temperature forecasts. Consider staying mostly indoors on very hot days. Need to get out with an older child? Consider your local library, a shopping mall, or other breastfeeding friendly locations - check out the pumpspotting app to find some near you! These are just a few quick tips but if you have any questions about staying cool this summer -- contact our lactations consultants and they can help! This post first appeared on the Breastfeeding Resource Center (BRC) website. With two locations (Abington and King of Prussia), the BRC offers consults and free classes to families in the Philadelphia area. For more information, please visit: breastfeedingresourcecenter.org Annemarie Nagle is a Board Member of the Breastfeeding Resource Center (BRC), a nonprofit corporation committed to providing expert clinical and educational breastfeeding services. Annemarie lives in Plymouth Meeting, Pa with her husband, their two year old daughter Amelia, and their dog Dutch.  As anyone whom has taken my classes knows, I rarely tell people what they need or should do. In fact, in the vast majority of birth-related situations, that goes completely against the scope of both childbirth educators and doulas. However, I will tell you this. A doula does not take the place of a birth class. So if you feel you need a doula for support and education, then you also need a birth class. 1. A birth class provides you with free-flowing education - the facts, the research, the risks versus benefits, the information necessary for formulating your own birth priorities - while a doula helps support you in putting it all into action based on your own expectations/desires. 2. The training and certification of a birth doula is completely different than that of a childbirth educator. A birth doula actively trains in listening, non-judgmental support, and verbal and physical comfort techniques while childbirth educators train in dissecting research, providing unbiased evidence-based information, understanding medical interventions and procedures, hospital procedures and policies, and public health. 3. If budgeting for a birth class and a doula proves financially difficult, many birth professionals will be flexible with payment, either working out a payment plan, a barter, or a discounted rate. Keep in mind that discounted services are generally reserved for those with a true financial hardship. 4. Prenatal doula visits are a time for you and your doula to get to know one another, to build a plan for your communication in labor, and to relate your birth wishes to the role of your doula in labor. Childbirth classes are a time for you to learn the physiology of the process and have a basis for why things may be suggested in labor and why your doula may be encouraging you to ask questions of your provider. 5. A birth class will help you take greater advantage of the skills and encouragement offered by the presence of a doula - you will literally be able to express a desire for certain techniques, verbal affirmations, or positions, and know what questions you should be asking and why - because your knowledge base will be far broader and more comprehensive than without the education component. We rarely have the responsibility in being both informed and confident when approaching such a transformational life event as we do in birth. The childbirth professional community, both locally and nationally, is vibrant and multi-faceted and has the potential to offer support in many ways, allowing you to build confidence and knowledge while being supported in putting it into practice. For more info, check out these blog posts on the differing role of a childbirth educator and a doula: Science and Sensibility Giving Birth With Confidence Here are two great pancake options - something a bit sweet and something a bit savory!
Check out the video post on Instagram @blossomingbelliesbirth! Whole Grain Pancakes adapted from "Vive Le Vegan!" by Dreena Burton *I double this recipe to feed three hungry kids! 1 cup whole wheat pastry flour 1 tbsp baking powder 1/2 tsp cinnamon 1/4 tsp nutmeg 1/4 tsp ginger 1/8 tsp sea salt 1 cup + 1tbsp unsweetened almond milk 1 tbsp coconut oil (melted) or canola oil 1 mashed banana 3/4 cup to 1 cup pureed pumpkin 1/2 cup nuts, berries, seeds, chocolate chips, etc. (optional) Toppings: coconut oil maple syrup or honey ground flax seed peanut or nut butter Whisk together all the dry ingredients. Place all the wet ingredients in the blender to mix or place in a bowl to mix with an immersion blender. Combine the wet and dry ingredients. Drop in 1/2 cup portions onto a hot griddle. Cook just until edges appear dry then flip and cook for another 1-2 minutes. Serve with any combination of the above toppings. * The pumpkin offers up Vitamin A, important for cell growth, immune function, and sight. The coconut oil is full of healthy fats, good for brain and eye function. The optional nuts and seeds offer minerals such as magnesium and zinc and protein to help in feeling full longer! Savory Chickpea Pancakes adapted from the blog "Oh She Glows" *I triple this recipe to feed three hungry kids! 1/2 cup chopped veggies (asparagus, broccoli, cauliflower, peas, dark leafy greens, shredded brussels sprouts - basically whatever I have on hand) 1/2 cup chickpea flour (also known as garbanzo flour) 1/4 teaspoon garlic powder 1/4 teaspoon sea salt 1/8 teaspoon freshly ground black pepper 1/4 teaspoon baking powder 1/2 cup + 2 tablespoons water For serving: salsa, avocado, hummus, tahini, cashew dressing, hot sauce, plain unsweetened yogurt (grassfed if possible) Sautee the veggies and set aside.. In a bowl, whisk together the dry ingredients. Add the water and whisk well. Add in the veggies. Drop in 1/2 cup portions onto a hot griddle. Cook just until edges appear dry (usually longer than a traditional breakfast pancake) then flip carefully and cook for another 1-2 minutes. Serve with one or a combination of toppings. *The chickpea flour is full of protein, necessary for organ function. The veggies offer a wide array of minerals important for bone density, tissue growth and strength, circulation, hair and nail growth, etc. depending on which combination of vegetables being used. Avocado and grassed yogurt offer healthy fats. Hummus, tahini, and cashew dressing offer more protein and calcium for bone strength and hair and nail growth. Who knew pancakes could be so good? Nothing says winter like Sunday afternoons spent in the kitchen with the smell of roasting onions and garlic. But I'm increasingly finding that, although I love these slow-cooking days, sometimes I need something a bit faster or something that will last us several meals. Here are two options that cover both those criteria. And they're delicious, nourishing, and warming.  Sweet Potato Macaroni and Cheese (vegan) *This is a variation of Super Creamy Mac and "Cheese" from www.veganyumminess.com 16oz. dried rotini 1 cup sweet potato, cut into 1/2 inch pieces 1/2 cup carrots, cut into 1/2 inch pieces 1/2 cup onion, roughly diced 1-2 garlic cloves, whole 3/4 cup water from the cooked veggies 1/2 cup coconut milk (full fat) 1/4 cup nutritional yeast 1-2 tbsp tamari 1 tsp salt 1 tsp turmeric 1/4 tsp garlic powder 1/4 tsp onion powder pinch red pepper flake (optional) two 16 oz. packages frozen broccoli or any combination of frozen veggies (mixed veggies, greens, etc.) Fill a large pot halfway with water and boil the sweet potato, carrots, and onion in a saucepan filled for about ten minutes, until soft. Using a slotted spoon, transfer the veggies into the blender; add 3/4 cup of the cooking water, the whole garlic cloves, and the remaining ingredients into the blender. Puree. Add more water to thin out the sauce if necessary. Using the same pot from the veggies, fill again with water. Bring to a boil and put in the frozen veggies; cook until soft. Strain. Fill the same pot again with water and cook the pasta according to the package directions. Strain the pasta into the same strainer as the veggies. Put the sauce into the pot and then the pasta and veggies. Toss and enjoy! (If you want to do this in fewer steps, you can use three different pots to cook everything simultaneously but I'd rather take more time and do less dishes but that's just me ;-) 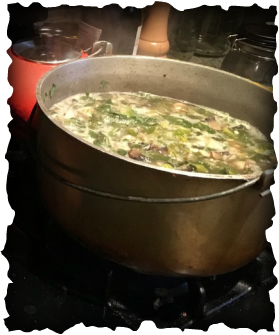 Mushroom, White Bean, and Greens Soup with Barley (vegan) 1 cup onion, diced 4 cloves garlic, diced 1 pound mushrooms (baby bella, shitake, whatever you have), chopped 1 cup white wine (or vegetable broth, water, red wine) 2 portabello mushrooms 1 bunch dandelion greens 1 bunch escarole 2 cans white beans (or about 5 to 6 cups) 1 tbsp tamari 1 tbsp ground sage 1 salt (or more to taste) 1 tbsp ground sage 1 tsp black pepper pinch red pepper flakes (optional) 1/4 cup nutritional yeast flakes (optional) or parmesan cheese (optional) about 6 cups water or vegetable broth (or water and two vegetable bouillon cubes) 1 cup barley In a large soup pot, sautee the onion and garlic for a few minutes then add in the mushrooms. When the mushrooms have shrunk in size and brown bits are just starting to stick to the bottom of the pot, deglaze with the white wine. Stir to scrape up the bits on the bottom of the pot. Add the greens, beans, tamari, seasoning, nutritional yeast flakes, and barley. Stir and cook for two minutes, watching to be sure it doesn't burn. Add the water. Bring to a simmer, turn down heat, and simmer for at least 30 minutes. Enjoy! I recently had the pleasure of being interviewed by a new childbirth educator as part of her certification process and, in answering her questions, realized how much they made me analyze my work and articulate my love for what I do. Check it out!
Tiffany: Why did you want to become a childbirth educator? Me: I wanted to become a childbirth educator after my first son was born and I realized how much information was not shared by providers to clients when planning for birth. The more I learned about the normal birth process the more I saw how divergent it was from mainstream conventional thought and that made me incredibly passionate about changing that inaccuracy and reframing the public opinion about birth to be more woman-centered rather than technology-driven (which does not mean promoting a certain model of birth, more so a model of care). T: What - to you - is the most challenging aspect of this profession? Me: I've been teaching for ten years and the challenges have varied along the way. Initially, the most challenging aspect was learning when to listen and not share because sometimes it's not the right space or time to give research-based info; sometimes women (and partners too) just need to be heard. More recently - not so much a challenge but more a consideration - I've been working on changing things up a bit in terms of the order in which I discuss topics and the dynamics of presenting information to keep the class fresh and engaging (for both myself and the participants!). T: Do you follow an organizations predetermined class or do you make your own class? Me: I am certified by Birth Works and the classes I teach are based on their philosophies. Birth Works is not a methods class and does not tell women "how" to give birth but instead provides women with the safe space to explore their birthing options and their own priorities while being supported in finding research-based information and developing tools for communication and empowerment. Working within and building upon these constructs, ideals, and guidelines, the classes I teach have become my own. I am a firm believer in the facilitator making a big difference in how effective the class is and feel passionately that there should be some leeway for facilitators to make the classes they teach their own while still respecting the philosophies of the organization with which they are a part. T: How many women do you work with a year? Me: Throughout my work in childbirth education, doula support, and breastfeeding support, I work with close to 200 couples per year. In childbirth education specifically, the number is probably around 175. T: Are there any resources, books, etc. that you have found particularly helpful to developing your practice? Me: I focus a lot of my work on pelvic bodywork and dynamics so one of my favorite books initially was "Let Birth Be Born Again" by Jean Sutton. A couple others that have had a huge impact on my philosophies include "Birth as an American Rite of Passage" by Robbie Davis Floyd and "Rediscovering Birth" by Sheila Kitzinger. I particularly love anthropological books on birth and the body; Sarah Blaffer Hrdy is one of my favorite authors. T: Why do you feel it is important for families to take CBE classes? Me: It is really important for families to take out-of-hospital childbirth education classes specifically so that they can receive an unbiased perspective on the birth process as well as learn communication skills, build confidence in understanding consent and refusal and in their rights, and develop their own ideas of what a positive birth experience looks like. In addition, gaining knowledge of options, learning tools for working through labor discomfort, and building a partner's confidence in him or herself as birth support are very important for creating an empowering experience. T: Based on what you have learned from your own experience, what advice would you give a new CBE? Me: My best advice for a beginning childbirth educator would be to create a non-judgmental space for women and their partners to open up about their feelings, thoughts, anxieties, expectations, and hopes for labor. This may have the most impact in empowering couples to come out of their births feeling really great as they haven't been forced to believe in something but have been supported in developing their own ideals. Also, remember that it is okay and incredibly important to always be learning as the professional. Honesty when not knowing the answer to a question in class is key and will help to build trust between the client and the facilitator and will allow the facilitator to grow as a professional. A big thank you to Tiffany Lynn Kennedy, Birth Arts International Trained Doula and Birth Arts International Trained Childbirth Educator for asking me about my journey. Find her online at www.birthwellnessdoula.yolasite.com and send her an email at tiffanylkennedy@yahoo.com.  Are you birthing in Philly and confused/overwhelmed/unsure about your options for place of birth and type of care provider? Look no further! Here is a comprehensive* list of all the options available to expectant families in the greater Philly area. Here’s to positive, healthy, and well-informed birthing! *There is surely a chance I have missed a provider or two here so please feel free to comment below with any additions! **Notice some options overlap depending on how it’s group so check out the whole list. ***CNM refers to a Certified Nurse Midwife; CPM refers to a Certified Professional Midwife; LM refers to a Licensed Midwife; a great resource for sorting through the differences between the certifications is here: [Photo of Tiff Hare and Family of Karma Birth Services] http://mana.org/about-midwives/legal-status-of-us-midwives [Photo by www.tammybradshawphoto.com] Hospitals Bryn Mawr Hospital (Montgomery County) Cooper Hospital (Camden NJ) Delaware County Memorial Hospital (Delaware County) Einstein Medical Center Montgomery (Montgomery County) Hahnemann Hospital (Center City Philadelphia) Holy Redeemer (Meadowbrook, Montgomery County) Hospital of the University of Pennsylvania (West Philadelphia) Inspira Medical Center Elmer (Elmer, NJ) Jefferson Health (Center City Philadelphia) Lankenau Medical Center (Wynewood, Montgomery County) Paoli Hospital (Paoli, Montgomery County) Pennsylvania Hospital (Center City Philadelphia) Riddle Hospital (Media, Delaware County) St. Mary’s Medical Center (Bucks County) Temple University Hospital (North Philadelphia) Virtua Hospital in Voorhees (Voorhees, NJ) Birth Centers LifeCycle Woman Care (formerly the Bryn Mawr Birth Center, Bryn Mawr, Montgomery County) The Birth Center in Wilmington (Wilmington, DE) Valley Birth Place (Huntingdon Valley, Montgomery County) Homebirth Midwifery Practices Inner Circle Midwifery, Asasiya Muhammad, CPM, LM Luna y Sol Midwifery and Family Wellness, Terri Simmons, CPM Midwifery Care Associates (NJ), CNMs Midwives of New Jersey, CNMs Midwifery Traditions, Kathy Hindle, CNM Motherland Midwifery, Christy Santoro CPM New Birth Experiences (NJ), Dina Aurichio CPM Rising Moon Midwifery, Kate Aseron CPM Urban Bush Baby Midwifery, Janeyne Sexton CPM Woman Wise Midwifery, Karen Webster CPM Waterbirth Gentle Beginnings, Inspira Medical Center (Elmer, NJ) Virtua OBGYN and Midwifery, Karen Shields, CNM, Virtua Voorhees (Voorhees, NJ) Valley Birth Place, CNMs (Huntingdon Valley, Montgomery County) The Birth Center in Wilmington (Wilmington, DE) *Waterbirth is an option when birthing at home In-Hospital Low-Intervention Birthing Suites Pennsylvania Hospital; jacuzzi tub available for laboring (not birthing) Hospitals with Midwives on Staff Bryn Mawr Hospital (Montgomery County) Delaware County Memorial Hospital (Delaware County) Doylestown Hospital (Bucks County) Einstein Medical Center Montgomery (Montgomery County) Hahnemann Hospital Hospital of the University of Pennsylvania Pennsylvania Hospital St. Mary’s Medical Center (Bucks County) Independently Practicing Midwives with Hospital Privileges Midwifery Traditions, Kathy Hindle, CNM (Einstein Montgomery Hospital, Montgomery County) Valley Birth Place Birth Center and Woman Care, Barbara D’Amato, CNM (Einstein Montgomery Hospital, Montgomery County) Woman Wise Midwifery, Ronni Rothman, CNM (Einstein Montgomery Hospital, Montgomery County) VBAC **VBAC options include hospitals with OB or midwifery care or homebirth in PA with CPMs Thank you to those who contributed their knowledge in making this list accurate and comprehensive - Christy Santoro, midwife Mari-Carmen Farmer, and Lori Daley of Delco Doula Birth Services.  'Tis the season...for the warming, invigorating, immune-enhancing tonic known as fire cider. For years, this potent medicinal food tonic has been used for it's antibacterial and immune boosting benefits. Variations on ingredients abound but the basics remain the same - a combination of foods and possibly herbs renown for their illness preventing and healing properties steeped in unfiltered apple cider vinegar for several weeks. The result is a potent tonic of which a spoonful can be taken daily for prevention or a tablespoon or two during illness. Not only will this strengthen your immune system but it's sure to put hair on your hobbit feet too. McCollum Family Fire Cider (makes enough for two quart jars) two bulbs garlic, smashed and chopped a generous dose (about a cup or so) of fresh grated ginger three to four jalapeños, sliced, seeds included about a cup of grated or chopped horseradish root a tablespoon or more of raw honey (optional) a quart and a half or so of unfiltered apple cider vinegar Split the ingredients between two quart size jars (any quart-size jars will do). Pour the apple cider vinegar over the ingredients in the jars, leaving about an inch of space at the top. Tamp down the ingredients and stir gently with a wooden spoon. Cap the jars and let sit for four to six weeks. Shake gently daily.  Whether you're stuck in a rut and looking for a few new ideas or just expanding your palate with a few different foods, check out the list below for some super nourishing and invigorating foods for pregnancy. 1. Chia Seeds: These tiny black and white seeds are chock full of calcium (to help reduce the risk of high blood pressure and pre-eclampsia, aid in the development of the baby's bones and teeth, and an aid to muscle contraction and enzyme and hormone functioning), protein, healthy fat, magnesium, and iron (WHO). Throw them into a salad, blend them in a smoothie, sprinkle them over yogurt or oatmeal. For a healthy treat, check out this Chia Seed Pudding recipe from one of my favorite food blogs, Oh She Glows. 2. Avocados: These fruits, native to Mexico and Central America, are well known for their high content of healthy fats but also contain a huge dose of vitamin C, helpful for strengthening the amniotic sac and boosting immunity, and vitamin B-6 as well as a decent amount of iron and magnesium and a bit of protein too (Casanueva). Go classic with guacamole, dress up a salad with slices, eat with scrambled eggs, or put into a wrap. Or check out this awesome vegan chocolate avocado mousse from MindBodyGreen. 3. Fermented Foods: It's hard to go anywhere now in a natural foods community without being bombarded with the benefits of a healthy gut flora. But it's true! The beneficial bacteria from fermented foods can help strengthen the immune system by reducing the presence of "bad" bacteria and help balance the production of stomach acid, reducing reflux and heart burn so common in pregnancy (Williams). In addition, fermented foods are high in enzymes for aiding digestion and reducing constipation, B vitamins for mental clarity, heart health, bone strength, good vision, high energy, and elevated mood, and omega-3s for brain and eye development in your baby (Whitaker). Saurkraut, miso, kimchi, kombucha, tempeh, yogurt, lacto-fermented pickles, and kefir are all great options and often simple to make at home. A great recipe for mason jar sauerkraut from The Kitchn can be found here. 4. Blackstrap Molasses: This by-product of the sugar refining process is a hidden gem of iron - for improving the oxygen-carrying capacity of blood, boosting energy, aiding the creation of DNA, and helping to prevent preterm labor and low birth weight ("Iron-deficiency anaemia") - calcium, vitamin B6, magnesium, and selenium. Drizzle a tablespoon over yogurt or oatmeal, mix into a smoothie, or eat by the spoonful. 5. Nettles: This amazing herb that grows wild all over sets the foundation for a healthy and well nourished pregnancy. Packed with iron, calcium, potassium, silica (a mineral crucial for growth and development of the bones, muscles, connective tissues, and ligaments), vitamin A, vitamin K - an important clotting factor in the blood, and anti-inflammatory properties (Wolf), it is great to drink as a strong tea or infusion throughout pregnancy (Weed). Steep a small handful of dried nettle leaves in boiled water in a quart mason jar, covered, for 30 minutes to four hours. Drink hot or iced and consume what's prepared within 48 hours. 6. Lentils: Just one cup of cooked lentils provides almost a full serving of folate, in addition to iron, copper, fiber, and protein ("Lentils"). Folate, the naturally occurring form of folic acid, is crucial for brain function, mental and emotional health, aids in the production of genetic material (incredibly important in pregnancy), and helps prevent neural tube defects. Lentil soup is a favorite in our house. Here's how we do it - give or take depending on what's in our frig. Hearty Lentil Soup Lots of garlic, chopped Lots of onion, chopped Carrots Celery A pound or so of kale or other dark leafy green, chopped Four cups of uncooked lentils Salt Pepper Thyme (fresh or dried) Basil (fresh or dried) A few bay leaves Turmeric (a healthy dash for it's anti-inflammatory properties) Water or vegetable stock, to an inch from the top of the pot Nutritional Yeast Sautee the garlic, onion, carrots, and celery until softened, about five minutes. Add in the kale, lentils, dried spices, and continue to stir for a few minutes. Add the water or vegetable stock. Bring to a boil and then reduce to a simmer, stirring infrequently. Once the soup has simmered for an hour or so, add in the nutritional yeast, and simmer for a bit longer. Sometimes we will use an immersion blender to blend the soup a bit once it has cooled, to create a thicker consistency. I often find I need to divide it up into two pots as well. Save some for the week and freeze the rest. 7. Citrus: These fruits have amazing health benefits ranging from reducing risk of stroke and cancer to boosting immunity, increasing nerve cell function in the eyes, and reducing stress ("6 Health Benefits of Citrus Fruits"). Just two clementines provide the body with about 70mg of the 80 to 85 mg of recommended vitamin C in pregnancy (which will aid in iron absorption if eaten with iron-rich foods) (Perinatology.com). Toss them into a salad or just keep them as a quick snack in your bag or in the car. 8. Raw Almonds: With your internal organs being squished up a bit higher to make room for your growing baby in addition to hormonal changes that relax smooth muscles and slow digestion, heartburn can fast become a reality for many pregnant people ("Heartburn in Pregnancy"). A small handful of raw almonds after every meal and snack can help alleviate this common issue as well as provide calcium, protein, healthy fats, and iron in the diet. 9. Pastured Eggs: Let me start with saying that a vegan diet can be completely healthy in pregnancy and there is not a need to consume animal products to grow a baby. However, if eggs are a part of the diet, understanding the benefits of pastured eggs versus conventional or even cage free eggs is important. Pastured eggs means that the chickens have been free to roam in the grass, complementing their grain-based diet with bugs and grasses, which increase the amount of Vitamin A and healthy fats in the eggs. Eggs are a good source of protein, iron, omega-3 fats, and vitamin A. The darker yellow the yolk, the higher the vitamin A content. Vitamin A supplementation in pregnancy is not recommended as it can increase the likelihood of birth defects but consuming vitamin A from food sources is a healthy way to increase immune function (Azais-Braesco). As protein requirements in the third trimester near 80 grams daily, adding eggs into the diet can be an easy way to get closer to the recommendation. Hard-boiled eggs as a snack or in a salad or scrambled eggs with greens in the morning are just a few ways you can incorporate them. 10. Dark Leafy Greens: And last but not least, my favorite all around food for health and vitality - dark leafy greens. Dark leafy greens are chocked full of antioxidants such as carotenoids (which help decrease the risk of cancer), vitamins such as folate, C and K, minerals including iron and calcium, fiber, and even protein (Adams). They are incredibly nutrient dense, meaning calorie for calorie, they top most other foods for the amount of nourishment they provide. Midwife, herbalist, and doctor, Aviva Jill Romm, recommends two big handfuls of dark leafy greens per day to aid in circulation. They are also huge helpers in decreasing the discomfort of heartburn, particularly when they are a consistent part of the diet. Herbalist Susun Weed recommends cooking greens well to ease the nutrient absorption; simmer them away in a soup where the broth will absorb any nutrients the greens themselves lose and the nutrients still left will be super easily broken down. In addition, the fat soluble vitamins in the greens will be more well absorbed if a bit of fat is eaten with them; sautee greens in some coconut oil or drizzle raw olive oil over them to maximize the absorption. Another great way to eat greens is to incorporate them into sauces - increase the nutrient density of pesto sauce by cutting back on the basil and adding spinach and a few leaves of kale or collards. The strength of the garlic and basil will overpower the bitterness of the greens and no one will be the wiser. Looking for a few more healthy foods to explore? Check out the benefits of coconut oil, raw honey, garlic, nutritional yeast flakes, flax seeds, and hemp seeds.
**This information has not been evaluated by the FDA. Please consult a nutritionist or your care provider for more information.** Sources: "6 Health Benefits of Citrus Fruits." Best Health. Best Health Magazine, 2015. Web. 23 Oct 2015. Adams, Ingrid. The Health Benefits of Dark Green Leafy Vegetables. Kentucky: University of Kentucky College of Agriculture, 2013. Print. Azais-Braesco V, Pascal G. "Vitamin A in pregnancy: requirements and safety limits." American Journal of Clinical Nutrition 71.5 (2000 May): 1325s-1333s. Casanueva E, Ripoll C, Tolentino M, Morales RM, Pfeffer F, Vilchis P, Vadillo-Ortega F. "Vitamin C supplementation to prevent premature rupture of the chorioamniotic membranes: a randomized trial." American Journal of Clinical Nutrition 81.4 (2005 Apr 8): 859-63. Elias J, Bozzo P, and Einarsonn A. "Are probiotics safe for use during pregnancy and lactation?" Can Fam Physician 57.3 (2011): 299–301. Print. "Heartburn in Pregnancy." Babycentre. Babycentre. June 2015. Web. 24 Oct 2015. "Iron-deficiency anaemia." Babycentre. Babycentre, April 2015. Web. 23 Oct 2015. "Lentils." The World's Healthiest Foods. The George Mateljian Foundation, 2015. Web. 23 Oct 2015. Perinatology.com. Focus Information Technology, 2010. Web. 1 Nov 2015. Romm, Aviva Jill. The Natural Pregnancy Book: Herbs, Nutrition, and Other Holistic Choices. New York: Celestial Arts, 2003. Print. Weed, Susun. Wise Woman Herbal for the Childbearing Year. Colorado: Informed Homebirth, 1986. Print. Whitaker, Dr. Julian. Dr. Whitaker America's Most Trusted Wellness Doctor. n.p., 2015. Web. 24 Oct 2015. WHO. Guideline: Calcium supplementation in pregnant women. Geneva, World Health Organization, 2013. Williams, Dr. David. Dr. David Williams Searching the World for Better Health. n.p., 2015. Web. 24 Oct 2015. Wolf, Nicki. "Nutrition of Stinging Nettles." Livestrong.com. Demand Media, 15 Sept 2015. Web. 24 Oct 2015. When we discuss fears of labor, one of the most common concerns that expectant parents bring up is a fear of tearing and it almost always elicits a cringe from partners at the mere mention. To think that such a sensitive area - already stretched in response to the emerging baby - has the potential of tearing to create more space is enough to make anyone's eyes roll into the back of her head. But there's a little known secret out there - tearing and episiotomies don't have to be the norm and actively minimizing perineal trauma is possible.
This amazingly resilient yet stretchy area between the vagina and the anus is called the perineum (the "taint" in more familiar terms). This fibromuscular structure is part of the pelvic floor and is known as the central tendon of the pelvis because many of the pelvic structures intersect here (Ritchie). Throughout the labor process and especially during the pushing phase of labor, the perineal area is flooded with blood and the hormones relaxin, which softens the ligaments and tissues, and progesterone which encourages smooth muscle relaxation. These hormones allow the area to stretch and become even more elastic to accommodate the baby's slowly crowning head. Let's do a quick anatomy lesson - get the lay of the land so to speak - so we can understand why minimizing or eliminating damage to the perineal area is a good idea and also why a natural tear is not always the traumatic thing we so greatly fear. If you're not so into the why, feel free to jump ahead a few paragraphs for the tips and tricks on reducing perineal damage. We'll begin with the basics of the pelvic floor. The three layers of muscle of the pelvic floor are responsible for keeping the structures above it, such as the bladder, uterus, and rectum, in place. The three layers are the superficial perineal layer, the deep urogenital diaphragm layer, and the pelvic diaphragm. (Beyond Basics). For our purposes, we will be discussing the superficial perineal layer, the group of structures providing support to and coming together at the fibromuscular mass between the vagina and the anus, called the perineal body. The perineal body or perineum anchors several muscles including the levator ani (helpful in providing support and function for the anal sphincter) and the external anal sphincter. The superficial transverse perineal muscle starts at the sit bones and connects to the perineal body, reinforcing the deep transverse perineal muscle to further stabilize the perineal body. The deep transverse perineal muscle, starting at the inner part of the ischiopubic rams and connecting to the perineal body and external anal sphincter, is responsible for keeping the perineal body in place as well as supporting the function of the levator ani and the urethra sphincter, which controls the flow of urine. The perineal membrane, a fascial thickening (connective tissue fibers) as opposed to muscle, starts at the pubic symphasis and attaches to the ischial spines, providing additional support to the perineal body (Ritchie). The bulbospongiosus arises at the perineal body, wrapping around the vagina, inserting at the clitoris (O'Rahilly). A great diagram of all of these muscles can be viewed at this link from www.netterimages.com. What is the take away from all this great info? The perineal area is pretty darn important when it comes to supporting the entire pelvic floor, vaginal, and anal region. So let's get an idea of why we should take good care of it. The Royal College of Obstetricians and Gynaecologists in the UK estimates that 85% of people with vaginal births will have some degree of tearing yet statistics from "Birth Matters: A Midwife's Manifesto" show that the rate of tearing at the birth center on the Farm in Tennessee, where midwives have attended close to 3000 births, is about 31.3%. As a unified nation, the United States does not have accurate statistics on tearing as standards for reporting vary from state to state. Perineal tears are classified into first, second, third, and fourth degrees. First Degree: the fourchette (where the labia minora meet at the perineum) and vaginal mucosa are damaged and underlying muscle is exposed but intact Second Degree: the posterior wall and the perineal muscles are torn but the anal sphincter is intact Third Degree: tear extends to the anal sphincter but the rectal mucosa is intact Fourth Degree: anal canal is opened and tear may spread to the rectum General complications from perineal trauma can include pain which can interfere with bonding and the establishment of breast/chestfeeding, increased risk of postpartum depression, infection, and even problems with fainting after urination and defecation (Tidy). Minor perineal damage from tearing can include extended healing time and discomfort from stitches and healing while complications from an episiotomy (a cut through the perineal area to enlarge the vaginal opening) can include longer healing time, more sutures, and a greater likelihood of third and fourth degree tearing. Third and fourth degree tears are associated with being more than twice as likely to experience fecal incontinence (Borello-France, et al.) with the potential of lasting five to ten years after birth (Evers, et al.). Tearing as compared to an episiotomy has a lower risk of posterior perineal trauma, lowered risk of needing suturing for perineal trauma, and lower risk of healing complications at seven days postpartum. The only disadvantage to tearing over having an episiotomy is an increased risk of anterior perineal damage. However, this research was done with laboring people in a supine (reclined) position which increases the pressure from the baby's head on the anterior perineum. In the 1970's, almost all vaginal births were accompanied by episiotomy without any research showing better outcomes; the research simply showed a lesser likelihood of tearing if an episiotomy was cut (let's think about that - if the area has already been cut, common sense would tell us that aside from the extreme of a third or fourth degree tear, the area is unable to tear because it has already been separated). It was standard to cut an episiotomy on first time parents and then on those whom had previous episiotomies, which adds up to about 100% of birthing people. The most accurate current episiotomy rates we have come from the UK, a country whose reporting standards are far more accurate and consistent from region to region than those of the U.S. According to the Royal College of Obstetricians and Gynaecologists (RCOG) guideline from 2007, rates vary greatly from country to country; episiotomy rates are 8% in Holland, 14% in the UK, 50% in the U.S., and 99% in Eastern Europe (Tidy). Rates also vary greatly from midwives to obstetricians, with 3.6% of midwives compared to 25% of obstetricians cutting episiotomies in the U.S. (American College of Nurse-Midwives). Now that we know some of the basics, let's get to the meat of it. What are some proven ways to lessen the chances of perineal trauma? Know Your Rights: It must be stated first and foremost that knowing one's rights in the laboring room is the most basic step in becoming an informed decision maker during the laboring process. Knowing your rights will help you build confidence in advocating for yourself and decreasing the likelihood of unnecessary perineal trauma. Check out a great list of your rights here. Nourish Your Body with Optimal Nutrition: "Good nutrition is vital to your body's work in preparing the perineum for stretching during birth. Hormonal changes during pregnancy cause the tissues of your cervix and perineum to become extremely thick and elastic. Crucial to this process is an adequate intake of protein, vitamin E, and short-chain fatty acids, which consist of two types of 'good' fat, Omega-3 and Omega-6. Short-chain fatty acids are found in nuts and seeds, cold-pressed oils, all types of beans, and fish such as salmon and tuna" (Griffin). Vitamin C intake is also helpful for increasing tissue health and elasticity so eating plenty of citrus, kiwi, peppers, broccoli, strawberries, cantaloupe, potatoes, and tomatoes can all help you reach your minimum 85mg daily recommendation (Vitamin C). Prenatal Perineal Massage: Massaging the perineal area once or twice per week for at least four weeks before labor begins has been shown by research to decrease the likelihood of episiotomies and possibly reduce the likelihood of tearing (Beckmann). However, it must be done past the point of burning and, as it creates small tears in the tissues, does have the potential for infection. In addition, the research shows that it mainly decreases the likelihood of episiotomies which brings up several variables that could influence the results (because the client has shown an interest in being proactive in reducing tearing/episiotomy, it would not be a stretch to suggest variables such as the client's choice of provider, client's discussion of prenatal massage with provider, and client's refusal of episiotomy all are at play). As midwife Gloria LeMay states "Advising a [person] to do perineal massage in pregnancy implies a lack of confidence that her tissues have been designed perfectly to give birth to her infant." So take this one or leave this one, whichever feels right to you. Second Stage of Labor Perineal Massage: Research suggests that a provider massaging the perineal area during the pushing phase decreases the likelihood of third and fourth degree tears as opposed to providers taking a "hands-off" approach. However, as stated in the meta-analysis done by the Cochrane Review, "hands-off" is a term that varies in it's definition from study to study (Aasheim) and the likelihood of third and fourth degree tearing without an episiotomy is very small (about 1%). It is also very important to note that these studies did not include any information about whether people had pain relief (which will decrease the amount of blood and hormones filling the perineal area and assisting with natural stretching), the position in which they birthed, and the nutrition of the participants during pregnancy. In addition, the type of lubricant used for massage may also have an effect on outcomes; vaseline or topical lubricant provides a slippery surface while food-grade oils such as coconut or almond oil are absorbed by the tissues and encourage elasticity. According to Simpson in her article "When and How To Push...", "No evidence suggests that manual massaging or stretching the perineum is beneficial, and many [people] find this technique uncomfortable." Hands-Off Providers: In an unmedicated birth, the perineal area is engorged with blood and hormones that encourage stretching and elasticity during the second stage of labor which means that in that scenario, any external increase in pressure or stretching (as in perineal massage by the provider) has the potential to increase the risk of bruising, swelling, and tearing (LeMay). Warm Compresses: A warm compress held gently against the stretching perineal area at the point of crowning can help reduce tearing (Aasheim). Avoid the Stranded Beetle: Also known as "keep your legs together!" The perineal area stretches side to side when the legs are kept open; this gives the area less ability to stretch front to back in response to the pressure from the crowning head. And keeping the legs from being pressed out side to side will actually create more space between the sitz bones, easing the baby's way out! Push Instinctively: Coached pushing keeps laboring people from listening to their bodies' natural inclinations to start or stop (Aderhold). A desire to "hold back" when the baby is crowning and emerging is actually a quite common and natural protector of the perineum (Reed). In addition, directed pushing may increase the likelihood of long term pelvic floor issues (Calais-Germaine). Embrace Your Ring of Fire: At this intense moment when the baby begins to emerge from the vagina and the perineal area begins to sting, the body is saying "Whoa! Slow down!" If you push right through this burning, the tissues don't have a chance to slowly open with the pressure from the baby's head. If you give little pushes or hold off - blow air out or do horse-lips - then the pressure from the baby's head will slowly stretch the area. Once it goes numb, if the area does tear, it is unlikely it would even be felt. In addition, according to LeMay, many people will instinctively reach down to support their baby's head at this point, further slowing the emerging and reducing the risk of tearing. Birth in an Upright Position: Multiple studies show that lateral and hands and knees positions decrease tearing and episiotomies while supine, squatting, and lithotomy positions increase the chances (Reed). However, squatting is a common position for birthing world-wide (Kitzinger); understanding the bones of the pelvis and their relationship to one another in creating space and stretching soft tissue is important....and brings us to the next point! Squat Optimally: If choosing to squat when the baby crowns, doing so in a way where the sacrum is lifted and the perineum directs towards the floor may decrease the risk for tearing as compared to a deep "resting" squat. More research needs to be done into the benefits of sacral nutation (forward tilting) on decreasing the likelihood of tearing. If you are interested in more discussion and demonstration of optimal positions for reducing discomfort in labor, decreasing tearing, shortening labor, and preventing baby position-related complications, check out the pelvic workshops I facilitate - Moving Through Labor for expectant parents and Creating Space for birth professionals! Change Position Frequently: Anyone who has heard me speak about easing the birth process, has heard me expound the benefits of frequent position changes (Balaskas). Changing the pelvic space allows the baby to make small head adjustments that can make for a more optimal position and smoother dilation and pushing stages of labor, all encouraging the smallest head diameter to make it's way out through the vaginal opening (keeping the perineal area intact!). The perineal area is such an important part of pelvic floor health and offers the amazing ability to stretch and become elastic for the birth of your baby! Understanding its complexity and how to keep the area intact and minimize perineal trauma is an important part of many people's birth priorities and should be knowledge that all birthing people take with them into their laboring space. Here's to happy and healthy perineums! *updated 2018* Sources: Aasheim V, Nilsen ABVika, Lukasse M, Reinar LM. "Perineal techniques during the second stage of labor for reducing perineal trauma." Cochrane Database Syst Rev. (2011): n. pag. Web. 27 Sept 2015. Aderhold, Kathleen J. and Roberts, Joyce E. "Phases of Second Stage Labor: Four Descriptive Case Studies." Journal of Nurse-Midwifery. Volume 36, Issue 5 (September–October 1991): 267-275. Print. American College of Nurse-Midwives. Midwifery: Evidence-Based Practice. 2012. PDF file. Balaskas, Janet. Active Birth: The New Approach to Giving Birth Naturally. Boston, Massachusetts: Harvard Common Press, 1992. Print. Beckmann MM, Stock OM. "Antenatal perineal massage for reducing perineal trauma." Cochrane Database Syst Rev. (2013): n. pag. Web. 27 Sept 2015. Beyond Basics Physical Therapy. "Anatomy of the Pelvic Floor." Beyond Basics Physical Therapy. 2015. Web. 27 Sept 2015. Calais-Germaine, Blandine. The Female Pelvis: Anatomy and Exercises. Eastland Press, 2003. Print. Griffin, Nancy. "Avoiding an Episiotomy." Mothering Magazine Summer 1995: 60. Print. Ina May Gaskin. Birth Matters: A Midwife's Manifesto. NY: Seven Stories Press, 2011. Print. Kitzinger, Sheila. Rediscovering Birth. NY: Pocket Books, 2000. Print. LeMay, Gloria. "Midwife's Guide to an Intact Perineum." Midwifery Today Issue 59 (Autumn 2001): Web. 12 Oct 2015. O'Rahilly, et al. Basic Human Anatomy. Dartmouth Medical School. Print. Reed, Dr. Rachel. "Perineal Protectors?" Midwife Thinking. Midwife Thinking, Mar 2015. Web. 27 Sept 2015. Ritchie, Laura. "Pelvic Floor Anatomy." Physiopedia. Web. 27 Sept 2015. Simpson, Kathleen Rice. "When and How To Push: Providing the Most Current Information About Second-Stage Labor to Women During Childbirth Education." The Journal of Perinatal Education. Web. 26 Aug 2018. Tidy, Dr. Colin. "Episiotomy and Tears." Patient. 16 Apr 2014. Web. 27 Sept 2015. "Vitamin C." National Institutes of Health. 24 June 2011. Web. 11 Oct 2015. |
AuthorAs the Philadelphia birth world blooms bigger and brighter, I think it's time I start putting some of the insightful questions I've received and information I've research into a public journal. I hope you'll find this inspiring, empowering, and totally enjoyable. Archives
February 2021
Categories |




 RSS Feed
RSS Feed