|
This week our focus is on induction! With our free webinar coming up live on Wednesday March 3rd, it seemed like a great time to review some common statements people hear from their providers and break down the evidence as well as the need to ask questions when faced with these comments because they may not be just as clear cut as they seem. We're not in a rush. It's okay if your induction takes three days. In ideal circumstances, this can be true. There are many factors though that may affect the induction timeline and be quick game changers, including - but not limited to - the water breaking prior to induction, back to back contractions that may limit the safety of other interventions, and pain medication that leads to more quickly increased Pitocin. Also, although this sounds good in theory, in reality, no one is eating well or resting well during an induction and that can lead to a quicker timeline of intervention acceptance or recommendation than previously planned. We recommend induction at 39 weeks. The ARRIVE trial (two great analyses are here: Parsing the ARRIVE Trial: Should First TIme Parents by Induced at 39 Weeks? by Henci Goer, BA and The ARRIVE Trial A Randomized Trial of Induction Versus Expectant Management by Rebecca Dekker, PhD, RN) has led to an increase in recommendation to induce low risk pregnancies in first time parents at 39 weeks. The circumstances of the families being induced in the ARRIVE trial are not recreated in every laboring room with every induction - a slow paced induction - and therefore one cannot expect the same results. In addition, the trial does not take into account those parents that have preferences for low intervention experiences. Consider the research (including average lengths of pregnancy) as well as one's own preferences when making a decision. Breaking the bag of waters can shorten labor. Research shows this to be true when it is done early in the induction process; research does not show a higher rate of cesarean birth or infection (however, known risk factors for increasing risk of infections such as frequency and number of internal exams must be taken into consideration). Breaking the bag of waters is not recommended if the baby is at a -2 station or higher and may carry a greater risk of complication depending on the position of the baby. Research does not show, in a spontaneous labor, that breaking the bag of waters reduces the length of labor. Induction doesn't increase the chance of a cesarean. The ARRIVE trial was so impactful because it was a large study and it refuted all the previous studies that had shown increased risk of cesarean with induction. However, as noted above, the circumstances of the ARRIVE trial are not recreated in most birthing places and therefore one cannot expect the same outcome. When comparing only induction of labor at different gestational ages, research shows an increased rate of cesarean birth with induction of labor with each week that passes. However, when comparing the cesarean rate of induction of labor with spontaneous labor in the same week - regardless of gestational week - research shows a lower rate of cesarean birth among the spontaneous labor group (however, one, of course, cannot "make" spontaneous labor happen so this is a bit like comparing apples and oranges). When making a decision about induction at certain gestational ages, it is important to consider as many risks and benefits as possible in the context of one's preferences to determine the appropriate choice at each gestational week for the individual. The risk of stillbirth almost doubles between 41 and 42 weeks of pregnancy. This statement includes both high risk and low risk pregnancies and is a “relative risk” statement. The statistical risk increases from 1.66 to 3.18 per 1000 births between 41 and 42 weeks of pregnancy (approximately .17 to .32 out of 100). This is approximately a 94% increase which sounds extremely high! However, when considering the numbers and not the percentage of relative risk, the numbers may not seem quite as alarming. The risk after 41 weeks of pregnancy for a low risk person ranges from .8 to 1.66 out of 1000 (.08 to .17 out of 100) based on the birth parent’s risk factors. It is important to remember that certain factors may change this risk (such as age of the birthing person) and also keep in mind that the induction process carries its own risks. Please remember the following when thinking about your choices and comparing them to what others may choose. As parents (and providers), we aim to minimize risk to our children as much as possible. For each person perceived risk may weigh differently in the decision making process. Each person deserves to be given the respect, the research, and the ability to make a decision that feels best to them, and after weighing the pros and cons (in their entirety including risks associated with every intervention and the path of no intervention) they also deserve to have their decisions respected without coercion, guilt, or fear of retaliation. The questions below can be used to have conversations with providers on any intervention related to birth or postpartum. - Brittany Sharpe McCollum, CCE(BWI), CD(DONA) is the owner of Blossoming Bellies Wholistic Birth Services, providing childbirth related services, classes, and workshops to parents and birth professionals in the Philadelphia area and worldwide. Sources:
Bhide Amarnath. Induction of labor and cesarean section. AOGS. Volume100, Issue 2, February 2021, Pages 187-188. Davey, MA., King, J. Caesarean section following induction of labour in uncomplicated first births- a population-based cross-sectional analysis of 42,950 births. BMC Pregnancy Childbirth 16, 92 (2016). Dekker, Rebecca PhD, RN, APRN, Mimi Niles, CNM, MSN, MPH, PhD student, and Alicia A. Breakey, PhD. Evidence on Advanced Maternal Age. Evidence Based Birth. March 29, 2016. Goldberg, Daphne MD, ABHM, FAAFP, Eva Zasloff MD. Artificial Rupture of Membranes. Integrative Medicine (Second Edition), 2007. Grobman W. A., Rice M. M., Reddy U. M., et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med 2018;379:513-23. Howarth G, Botha DJ. Amniotomy plus intravenous oxytocin for induction of labour. Cochrane. 23 July 2001. Muglu, J., Rather, H., Arroyo-Manzano, D., et al. (2019). Risks of stillbirth and neonatal death with advancing gestation at term: A systematic review and meta-analysis of cohort studies of 15 million pregnancies. PLoS Med 16(7), e1002838. Sun Woo Kim MD, Dimitrios Nasioudis MD, Lisa D.LevineMD, MSCE. Role of early amniotomy with induced labor: a systematic review of literature and meta-analysis. American Journal of Obstetrics & Gynecology MFM. Volume 1, Issue 4, November 2019, 100052.
1 Comment
Blossoming Bellies and Brittany Sharpe McCollum do not endorse any of the following companies or products. Any links offered in the email are affiliated with the author of the post, not affiliated with Blossoming Bellies Wholistic Birth Services or Brittany Sharpe McCollum. During the transitional fourth trimester, lots of changes are happening in your body and mind. While the baby’s well-being may be at the forefront of your mind, it’s important to prioritize your own physical and mental health during this crucial stage. A new parent may not see a clinical provider for up to six weeks after childbirth, and the body needs some TLC. Staying hydrated, maintaining a healthy diet, and taking advantage of the support of family and friends will be fundamental to regaining strength. Your core muscles have done a lot of hard work to grow and bring your baby into the world. Ligaments that have stretched and softened are now beginning to shrink and firm up. Your center of gravity has shifted again, and your posture is being impacted by all the time spent lifting and holding your baby. Maintaining good posture is particularly difficult in the postpartum period because of the lack of core strength in the first several weeks. Your abdominal muscles need a chance to stabilize and come back together to form a strong core. The good news is there are plenty of ways to support all of these changes during the postpartum period. Postpartum Exercise I get lots of questions about how and when to exercise after having a baby. I always recommend the 5-5-5 activity rule for my clients after the birth of their baby: 5 days in bed, 5 days around the bed, 5 days around the house. Your body has been working so hard for the last 9 to 10 months and needs time to recover! Generally speaking, about 2 weeks after an uncomplicated vaginal birth is a good time to start incorporating daily practices like breathing exercises, pelvic tilts, Kegels, walking, and arm/shoulder stretches. Exercise can be a great way to help strengthen and tighten stretched out muscles, improve or correct diastasis recti, and help get you back into the swing of things. Diastasis recti is the separation of the muscles along the middle of the abdomen that happens naturally during pregnancy to make room for a growing baby. A thin line of connective tissue called the linea alba lies between the two rows of the abdominal muscle and it stretches to allow the muscles to pull apart. giving birth, often the connective tissue will shrink and tighten up, pulling the muscles back together. While the condition sometimes corrects itself, other times it needs special attention. There are plenty of online programs that are geared towards helping improve or fix diastasis recti. If you are less than 6 weeks postpartum, I recommend working on not breathing into your belly (your ribs and chest should move more with each breath and your belly should not move much at all) and maintaining good posture while you are sitting and bending over, as these simple habits encourage a strong core. Maternity Compression The use of a postpartum recovery garment during the initial postpartum period is also super helpful in bringing your abdominal muscles back together and encouraging good posture. Many people are familiar with some form of maternity compression, like pregnancy support bands and compression socks. They may be less familiar, though, with how compression can help support the postpartum body. Like a pregnancy support band, a postpartum recovery garment provides gentle compression to the core but extends to encompass the upper thighs, posterior, and the top of the abdomen as well. Postpartum recovery garments should not be confused with shapewear or Spanx. Shapewear is designed for side slimming, not for providing support to your abdominal muscles after you’ve had a baby. During the postpartum period, side slimming garments put an increased pressure on the pelvic floor. Your pelvic floor has been relaxed and stretched during pregnancy. It is not in any condition to support an increased workload, as this can lead to prolapses and hernias. A postpartum recovery garment supports your abdominal muscles, stabilizes joints, and encourages your organs to settle back into their normal positions. Seeing as you now may be hunched over for a good portion of the day as you feed and care for your baby, your posture can suffer. As your muscles and ligaments firm back up, compression can ensure your spine is in proper alignment while that happens. You’ll be setting yourself up for better posture—and fewer aches and pains. There are a few considerations to keep in mind when wearing a postpartum recovery garment: ● Don’t wear the garment too tightly. It should not hurt or be difficult for you to breathe normally. Gentle support is what you’re aiming for! ● Don’t forget the importance of keeping good posture throughout the day. ● Check to see if maternity compression may be covered by your insurance provider.  Rebekah Mustaleski is Compression Director with MotifMedical.com and a Certified Professional Midwife with Roots & Wings Midwifery in Knoxville, TN, where she promotes evidence-based maternity care for families seeking an out of hospital delivery. She is working to improve maternal outcomes during the childbearing year and to promote a sustainable business model for midwifery practices across the country. Rebekah is co-owner of Roots & Wings Midwifery, LLC as well as Treasurer for the Tennessee Midwives Association. The physical and emotional aspects of pregnancy occur on a spectrum ranging from elation and pleasure to anxiety and discomfort, often embodying contradictory sensations at the same time. Anxiety has a way of creeping into even the most blissful moments and can affect the choices someone embraces, the way a person views their upcoming birth, and the ease with which they move through pregnancy.
According to a study in the Journal of Affective Disorders, as many as 20% of people experience antenatal depression and anxiety, with the incidence of anxiety rising in pregnancy. (This number, however, is difficult to use as a true guideline as it is suspected that antenatal depression is one of the most under-diagnosed and under-treated conditions.) These feelings can occur as a result of many factors including but not limited to bodily changes, shifts in physical ability, fear of loss, unanticipated complications, financial concerns, and hormonal changes that affect chemical release in the brain. High levels of anxiety are associated with increased likelihood of preterm birth, preeclampsia, and low birth weight as well as stalls in labor and distress during birth. Managing stressors and decreasing feelings of anxiousness may not only benefit one’s own daily life but can quite literally benefit the labor process and the baby too.
Pregnancy offers a unique opportunity to explore reactions to the world, to grow as a person, and to impact the long-term health oneself and their child. Recognizing areas in which one can take control and create calm is one of the first steps in embracing an empowered childbearing experience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4879174/ Postpartum recovery is a crucial stage. As new parents, you may think that the laborious period ends after your baby's birth, but this fantasy is not often the case. Usually lasting for six to eight weeks after delivery, the postpartum period requires you to devote utmost care and attention to yourself as your body adjusts. If not taken seriously, postpartum health can influence your lifetime risk of disease. Medical experts from Maryville University explain how chronic illnesses are on the rise, typically brought about by poor diet choices and lifestyle decisions. These can easily escalate to more serious health complications, especially for new moms. Well Seek note how a postpartum mom’s body may be depleted of the necessary nutrients due to ensuring that her baby’s needs are met. If a new parent doesn’t replace the nutrients with food from a healthy diet they increase their chance of chronic illnesses, infections, and mental health issues like depression. These will also affect them long after giving birth. More than anything, nutrition is your first line of defense and the key to regaining your strength. That said, here are some tips to plan your meals for postpartum recovery. Choose nutrient-rich foods By now, nutrient-rich foods should already be a staple in your diet, but even more so when you're in recovery period. Because your aim is to heal your body, nutritious foods are great because they also fight off inflammation. Ensure that you're getting a good mix of vegetables, fruits, yogurt, some whole grains, bone broths, healthy fats, and more. Check out our post ‘This is Your Birth’ for a list of pregnancy-friendly food, which you can consult after giving birth. Eat enough calories Calorie counting only comes second to making sure you're having a balanced diet. But if you're looking for a safe estimate, most doctors will recommend a daily caloric intake of 1,800 to 2,000 calories a day for postpartum parents. Of course, this can still vary depending on your prior weight and other factors. If you're breast-feeding, health writer Erin Coleman suggests adding an extra 400 to 500 calories a day to maintain your energy levels and keep your milk supply steady. After all, breast-feeding can burn as much as 500 calories. Consume more protein Protein is your body's building blocks. Without it, your enzymes, body tissues, and hormones will not be able to function normally. And after sustaining your baby's growth in your womb for months, it's absolutely essential to restore your sources. As a rule of thumb, your goal should be to have at least five servings of protein daily, but be sure to keep it high quality. Stick to foods like red meat, chicken, beans, and eggs. Always hydrate Hydration is standard for everyone, but it is important that postpartum parents drink even more water. Instead of capping your glasses at 8, aim to drink at least 10 to 15 glasses of water everyday. This is required not just to quench your thirst, but also to ensure you can produce enough breast milk. Moreover, consuming more fluids can speed up the repair of your regenerating body systems. Think collagen Not just an ingredient in your skin care products, collagen is a superfood that helps with the regeneration of tissues. Again, this is essential for healing bodies. Fortunately, you can find collagen in foods like egg whites, oranges, berries, and a variety of nuts. A study by the International Journal of Women’s Dermatology shows how collagen can even help with postpartum hair loss. Don’t be afraid to take supplements More than anything, you should be able to get all your required nutrients from food. But if you're struggling to keep up with your body's daily needs, you may want to enlist the help of supplements. Vitamin C, D, and Omega 3 are staples, but it's always best to consult with your doctor or healthcare professionals before trying anything.  Health and financial blogger Mya Summer believes that your diet is what dictates not just your outlook but also your capacity for enjoying life. When she’s not teaching yoga and tai chi at the local gym, she goes on forest hikes with her husband Timothy and their two huskies, Daniel and Vito. Over time, humans went from giving birth unmedicated to placing parents-to-be in a sterile environment, isolated from loved ones, with the fear of their impending labor looming over them. This type of birthing experience tended to enhance the parent's anxiety and induce more stress than was necessary. Stress-filled labor can lead to birth complications and a negative experience for both parent and infant. Fortunately, the medical community has come to realize that the benefits of doulas to a parent's birthing experience are far more significant than they realized. An expectant parent with doula support benefits significantly from having full emotional and physical support during a time in their life that may make them feel out of control. This type of support offers the self-confidence needed to have uncomplicated labor. Doula supported parents report experiencing less pain during delivery as well as a lower rate of epidurals, cesareans, and the use of medical instruments during the birthing process. This type of delivery also means that doula supported parents have lower hospital costs. Stress-free labor is highly beneficial to not only the expectant parent but the infant as well. Studies have shown that babies born from a doula supported birth have higher Apgar scores. There is also a positive parent-infant interaction during childbirth, which also results in boosting early breastfeeding scores. The overall experience provides the new parent with higher self-confidence in their abilities to bring their child into the world safely. Both the scientific and medical community now back doula support for birthing parents. Many studies and findings prove that this type of support has many benefits to both the parent and child that can't be ignored. WeTheParents have compiled these findings into 17 evidence-based benefits of doula support demonstrating the importance of doulas.  Neve is the mother of three, a natural birthing advocate, and a research nerd. She is chief editor at WeTheParents where she routinely creates engaging summaries of the scientific literature on various aspects of pregnancy and parenthood. You can catch her on Twitter and Facebook. Back to school! That time of year that students dread that can be surprisingly fun as they get to see the familiar faces they missed over the summer. The change can be a shock to everyone’s system. However, there are steps you can take to ease the transition back to school. Get Good Sleep Inadequate sleep hampers anyone’s ability to learn – let alone that of children who need to learn intensively. A lot of people don’t realize that children need 10 hours of sleep a night. Encourage good sleep and set a good example. Don’t use electronic devices in your bedroom, and have your children shut theirs off at bedtime. You may want to invest in blackout drapes if their bedrooms get a lot of sun. Getting up with the roosters may not be the healthiest thing for your children. Work With Your Child to Relieve Stress Many children get anxious before going back to school, but you can work with them, so they learn techniques to manage this stress. Train them in self-talk techniques. This will help them become less anxious.Take your child to the school grounds before the first day of school, so they can ease back into the environment. You can visit the classroom or playground. Schedule a play date with some of his or her classmates. This will help your child ease back into school and look forward to seeing friends. Take Part in Orientations This is an extremely important step if your student is new to a school. Just knowing how to get around the building will help relieve anxiety. And your child will get to meet his or her teacher, see the classroom, and get a feel for what the school year will entail. Purchase School Supplies This is one back to school activity that many children actually enjoy. Getting new school supplies! Take advantage of the many sales to stock up for what your children will need to take with them to school and what they will need to do their homework. Buy a new backpack and fill it with the items needed for school as you buy them. Most schools have a list of supplies the children should have, so be sure to print that out and bring it before you go shopping. (Some large stores may have the lists for the major schools in your area.) And don't forget to label major items like backpacks and lunchboxes, so they won’t get lost at school. Set Up a Workspace at Home Your child should have an inviting place to work at that he or she can use efficiently. The days of doing homework sprawled out on a bed are long gone! A younger child may want to be near you, so consider a section of the kitchen table or part of the family room. Older children are more likely to want privacy, so set them up in an office or bedroom with plenty of lighting and a comfy chair. Krista Harper is a freelance writer from Southern California and mother of two adorable young kids. She regularly covers lifestyle, beauty, and health related topics. Kritsa is always looking for ways to better herself and has a passion for helping families create balance and happiness in their lives.
Several months ago, I came across the most poignant of memes. Robin Williams from the movie Jumanji - disheveled and scraggly with the title "After Putting the Kids to Bed..." and the caption "What Year Is It?" I know I'm not alone in feeling like bedtime is a time warp in which two hours can often get lost in snacks and trips to the bathroom and toddlers abruptly in desperate need of water. And this is exactly why I was so excited to have Stephanie offer some tips for getting through this challenging time of day. - Britt Establishing and customizing a bedtime routine for your new baby can be a little tricky, and sometimes quite perplexing. Every child is different, and you will need to work with your baby’s individual sleep requirements. However, it’s best to develop a routine that is consistent. Read on about how to build the framework for an effective bedtime routine. How Much Sleep Does My Baby Need? Working with your baby’s sleeping habits is not a clear-cut process because the amount of sleep needed and when it is needed varies by age and by the unique needs of your child. However, here are some general guidelines of required sleep in a 24-hour period, organized by age group and based on a 2015 study conducted by the National Sleep Foundation. Newborns: 14 – 17 hours Infants: 12 – 15 hours Toddlers: 11 – 14 hours Preschoolers: 10 – 13 hoursRemember that these are just averages. Every child is somewhat unique when it comes to sleep patterns, so don’t be alarmed if your little one doesn’t fit perfectly into these guidelines. Prepare For The Worst Be prepared for what may happen after you’ve tucked your child into bed. From teething to nightmares, you and your child are bound to face sleep disruptions together. Here are a few common sleep challenges to be aware of: Newborns Colic Jaundice Infants Leaps Sleep Regressions Teething Ear Infections Early Childhood Bed-Wetting Nightmares Night Terrors Battling the Bedtime Tantrum Children love to test boundaries, which makes it important for parents to establish firm rules and limits at a young age. Unfortunately, the cutest age is also the age where tantrums are most prevalent (1-3 years old). But don’t worry, here are a few helpful tips to help you deal with tantrums like a pro: Positive Reinforcement: Make sure your child is rewarded for good behavior. Soon they will be able to spot the difference between behaviors that are rewarded versus those that are not. Give Them Choices At Bedtime: Maybe your child doesn’t want to go to bed, but chances are they will want to pick out the pajamas they wear, the flavor of toothpaste they use to brush their teeth, or their bedtime story. Add some diversity so that they are excited for bedtime, instead of treating it as a chore. What NOT to Do: Do not reward your child’s tantrum by giving in. Sometimes it’s easier, and a time saver to avoid the headache of arguing with your child, however this will only prove to your child that the tantrum was effective and increase the likelihood of it happening next time. Basic Components of an Effective Bedtime Routine Now that you have a general idea about how much your baby should be sleeping and some challenges you may face, here is an outline of a generalized bedtime routine. Food: Regardless of whether you’re formula feeding, nursing, or chasing around a toddler, you’ll want to fit in a feeding or snack at bedtime. However, not all kiddos do well with going to sleep with a full belly because they get gassy. Experiment with what and how much you feed your child before bed to find what works best for them. Books: This component will vary depending on your child’s age. With infants, it’s usually best to read the same book every time. This doesn’t need to apply during the day, however. Sticking to the same book at bedtime will help your baby’s brain recognizes that it’s bedtime. Potty: Although this one may seem obvious, it is often overlooked by parents after their busy day. Ensure that your child takes a trip to the restroom right before bed. They should soon pick up on this habit and initiate it on their own. Teeth: You can actually start this habit before your baby even sprouts teeth by brushing their gums gently with a silicone training toothbrush or a regular one with very soft bristles. This isn’t strictly necessary, but once your child begins teething, it’s important to make this habit part of their bedtime routine. Lullaby/Prayer: For this component, choose a song or songs that are meaningful to both you and your child. As with books, stick to the same songs or prayers, and keep them quiet and uplifting. Hopefully, following these guidelines will help you and your child establish a bedtime routine that really works. Remember, you can customize your bedtime rituals to meet the unique needs of your child. However, it’s best not to change things up on a nightly basis. Happy sleeping!
Author's Note: In no way is this meant to be a fully comprehensive outline of injustices nor is it intended to prioritize one form of injustice or the related trauma over another (as trauma is a lived experience; its effects are subjective and cannot easily be quantified by a third person). It is merely intended to shed light on some of the deeply entrenched inequities of birthing in a system that often fails to adequately meet client's needs on an individual basis. The year 2018 has been referred to as "The Year of the Woman" and for good reason. According to the New York Times, the historic political victories, the #metoo movement on social media, and the rising up, regardless of outcome, to make one's voice heard against patriarchal and fear-based systems have all led to a year of progress for women and minorities. However, one incredibly pervasive aspect of personhood, an area that is often thought of as female yet includes the queer, non-binary, and transgendered community, is childbirth. Labor and birth have continued to be riddled with both subtle and overt abuse, injustice, and disparity that is often overlooked. Birth and the transition into parenthood affects millions of people in the United States every year. The sensuality and vulnerability of this transformative time in one's life makes it an easy target for the implicit bias, condescension, lack of respect, and paternalism that can lead to trauma for both those experiencing and those witnessing labor and birth. Despite the pervasiveness of these qualitative deficiencies and the impending challenges of rising above and moving forward, change is possible and is already underway in many capacities. According to doula and DONA founder, Penny Simkin, "A birth is said to be traumatic when the individual ([birthing person, partner], or other witness (8)) believes the [birthing person's] or [their] baby’s life was in danger, or that a serious threat to the [birthing person's or their] baby’s physical or emotional integrity existed." Between 25 and 34% of people describe their births as being traumatic (Simkin). Risk factors associated with the perception of birth as traumatic include unexpected complications, unwanted routine interventions, lack of understanding or agreement over reasons for intervention, loss of control over sensations, perceived poor treatment, lack of respect, and lack of communication from staff, poor family support, personal defeat, and profound opposite of expectations. There are some factors that one can only, at best, hope to mitigate with support. Yet there are other factors over which providers have a profound impact - such as reducing the perception of poor treatment, thoroughly communicating with the laboring person and support people, and ensuring complete respect for the person and their legal right to informed consent and/or informed refusal. The intersectionality of racism, classism, sexism, and paternalism that occurs in childbirth is the perfect storm for a traumatic experience. From April Dawn Reigart, Integrative Nutrition Health Coach: One of the most poignant analogies of which I have come across is that of comparing one's first birth to one's first sexual experience. This comparison can be recognized by any birth-watcher, someone whom understands the intensity, vulnerability, and deep emotions that make up the labor experience (this does not necessarily refer to anyone whom attends birth but instead refers to someone whom is commonly present throughout the entire labor process). It refers not to someone whom is more comfortable managing the process but someone that is most comfortable simply being present. Let's take a moment to think about this. When someone is opening themselves up to a partner for the first time, what would they need to do feel most comfortable, confident, and in control throughout the experience? The list could be quite long but guaranteed it would include a partner that is patient, understanding of the wide variation of normal in the body's appearance and in the primal responses that are results of physical sensation, and respectful of the importance of ongoing consent and the boundaries set along the way. Respect may come in the form of communication, intuition, and a willingness to be flexible and adjust as necessary. These same things that someone needs to feel empowered and excited and positive about their first sexual experience are the things someone needs to feel empowered and excited and positive about their first (or second or third or fourth...) birth experience. People of color birthing in the United States have a three to four times higher perinatal mortality rate than non-Hispanic white women (and 12 times higher in New York City). Neel T. Shah, assistant professor of obstetrics and gynecology at Harvard Medical School, obstetrician-gynecologist at Beth Israel Deaconess Medical Center in Boston, and Director of the Delivery Decisions Initiative at Ariadne Labs, has pointed out that the maternal mortality rate for women of color is not only due to a lack of resources but is also due to the lived experience of being a person of color. He has cited the perpetuation of myths in obstetrics surrounding the perception of pain among women of color as being largely responsible for the mistreatment and subsequent greater morbidity and mortality among black women in the United States (Deborah Kuhn McGregor's book "From Midwives to Medicine: The Birth of American Gynecology" details the early days of obstetrics and its origins in brutality towards women of color and immigrants.) It is well understood that black women die at a higher rate in childbirth regardless of education, income, social standing, profession, or prenatal education (Lost Mothers). The racism, however subtle or pronounced, that people of color experience on a daily basis increases the likelihood of pregnancy-related complications. According to an article by Theresa Chalhoub, senior policy analyst for the Women's Health and Rights Program, and Kelly Rimar, women's health and rights intern, both at the Center for American Progress, "Racial disparities in risk factors related to pregnancy—such as hypertension, anemia, and gestational diabetes—exist and are exacerbated by stress related to racial inequality and often inadequate health care, which is not in tune with African American women’s needs." The increased nervous system response to moments of stress, fear, or discrimination, a biologically intended protective mechanism similar to "fight or flight", can prove debilitating when this increased response is happening on a frequent basis and the effects accumulate over many years. According to the documentary, "Expecting Possibility, "Stress is linked to one of the most common and consequential pregnancy complications, preterm birth." Black infants are twice as likely to die as white infants, a greater racial disparity in infant mortality than in the year 1850 (Villarosa). In addition, a 2016 study done by the University of Virginia found that "White medical students and residents often believed biological myths about racial differences in patients, including that Black patients have less-sensitive nerve endings and thicker skin than their White counterparts.” Reading this, especially as a black person preparing to give birth, may feel especially discouraging and frightening. However, there are ways to help mitigate the consequences of this reality and alter the course of a pregnancy, birth, and parenting experience. How does someone - anyone - up against such hard truths as these create an environment in which they maximize their health and minimize the effects of daily stress? Focusing on the aspects of care that one can control is a crucial part of mitigating the effects of stress. According to Miriam Zoila Perez, doula turned journalist, some ways to reduce the effects of stress in pregnancy include having a strong social network, prioritizing health and nourishment, asking for help when it is needed, talking through events that increase stress response, and daily meditation. Family, friends, and community can provide an outlet to discuss daily occurrences, surrounding oneself with love and fellowship, and decreasing the release of stress hormones in favor of increasing feel good hormones. Utilizing resources such as childbirth education classes, community doula programs, and infant care and postpartum preparation classes can decrease anxiety specifically surrounding pregnancy and parenting and help build networks of support throughout the childbearing year. It is important to recognize, however, that the root of racial bias and its effects on reproductive care are systemic and responsibility must be taken by the greater culture of white privilege and by those within the system that are perpetuating myth and providing unequal care - whether knowingly or inadvertently. According to Shah, "The common thread is that when black women expressed concern about their symptoms, clinicians were more delayed and seemed to believe them less." To truly reverse the trend of abhorrent mortality rates among people of color, the implicit bias, the racial stereotyping, and the paternalism that infiltrates daily life and reproductive care must be addressed. As Natalie Krichten, Pittsburgh based doula and owner of Growing Love Birth Services, suggests in her essay "Self Care and White Privilege," looking to leaders in communities of color whom are already doing the work of combating unjust care and empowering individuals may help a Eurocentric birth world to become a safe place for all whom are birthing in the U.S. Supporting businesses owned by people of color, spreading awareness about events such as the Black and Brown Maternal Health Fair being held June 8th 2019 at the Kingsessing Recreation Center, and connecting birthing people of color to health and wellness resources run by people of color can help to increase access to care, mitigate stress, and decrease morbidity rates. In an article written for Patient Safety and Quality Healthcare, author Megan Headley discusses the Maternal CARE Act proposed by senator Kamala Harris which provides grant money to the development of evidence based implicit bias training for health care workers, with a priority on OB/GYNs. The bill proposed by Harris also requests that the "National Academy of Medicine complete a study in bias recognition, with the goal of developing recommendations within three years for rolling out bias training to all medical schools and health programs" (Headley). From Pittsburgh birth worker Natalia Krichten, owner of Growing Love Birth Services: Society has seen a transition, in the last several decades, from families with two heterosexual married parents (which are now the minority) to a rise in co-habitating non-married parents and single motherhood, followed by gay families, multigenerational families, and trans gendered families. (Although I'd also like to take this moment to stress that babies born out of wedlock did not always carry stigma; prior to industrialization, capitalism, and the spread of Puritanism in the 16th century, children were absorbed into the mother's community. Their inheritance would have been affected by birth out of wedlock but they did not suffer the stigmatization that became prevalent in the 1500s. But that is a topic for another blog post...) Married mothers tend to be older and are disproportionately white and college-educated (Mathur) but married mothers are not as prevalent as they were fifty years ago; 40% of babies are born to unmarried mothers in the United States (this statistic does include those that may be co-habitating) (Italiano). The paradox is, however, that the restructuring of the traditional family sheds brighter light on the lingering and prevalent cultural bias towards people that are unmarried, particularly unmarried single parents of color. The cultural bias assumes single parents will provide incomplete parenting or a "lesser" parenting and that children will suffer, that single mothers will be less likely to pursue their own success, and that black women will be negligent and black fathers will be deserters (let me point out here that years of research has concluded that hands-on parenting is similar among dads of all races and the CDC has found that black fathers are more involved with their kids on a daily basis than dads of other racial groups (Culp-Ressler). These assumptions lead to discrimination and judgment both before, during, and after childbirth. When hearing this type of information, people often fall into two camps - those that have lived the experience of this judgment and those that quickly put up a wall and attempt to convince themselves that they don't have this bias (and to be fair, there are also many people whom take a moment to reflect upon this and do their own work in recognizing and moving past implicit bias). It is hard to hear but these unfounded allegations - no matter how nuanced - exist and begin long before pregnancy, affecting the way people both pregnant and giving birth are viewed, and following into their parenting journey. From Iris Kimbrough, CLC, Doula, and founder of Phoenix Rising Birth Works: Underlying judgment, coming from implicit bias, contributes to the paternalism that affects perinatal care. Paternalism is defined as "the policy or practice on the part of people in positions of authority of restricting the freedom and responsibilities of those subordinate to them in the subordinates' supposed best interest" (Paternalism). The first requirement in a paternalistic reality is the creation of a hierarchical system that places the provider at the top and the client at the bottom (see below for ways to upend this hierarchy and retain authority in a vulnerable position). When the provider holds the power in the situation - whether that power comes from the setting, a medically complicated situation, or the use of exclusive language not understood by the client - the client is automatically moved lower in the hierarchy and it becomes easier for them to assert that power. Examples of the assertion of paternalistic power plays include the insistence of internal exams in general and at specific intervals, the recommendation for labor augmentation in a non-emergent situation without a conversation leading to the opportunity for informed consent or refusal, the laying out of options that only include those preferred by the provider, hushed discussion with other providers in the vicinity of the person about whom they are talking, the pulling aside of partners or support people to persuade them to encourage the laboring person to make a certain decision, the use of fear and/or ultimatums to accomplish a specific end goal, and the use of intervention, touch, or examination without client consent. And this list goes on and on; these are only a few examples. It is every person's legal right to give informed consent or informed refusal at every step of the way when it comes to medical decision making, with the possible (not pre-determined) exception of a true imminent emergency (McCollum). From clan homemaker, idea cultivator, and tea drinker, based in Northeast Philadelphia, frequenting cafes and kitchen tables, beaches, and distant shores: Perhaps the most glaring example of paternalism in birth can be seen in the experiences of teen parents. Births among adolescents ages 15 through 19 have declined over the past 25 years and are at an all time low in the United States, accounting for 5% of all births in 2017 while a national survey of adolescents found that 77% of teen births are unplanned (Office of Adolescent Health). When the planning of a family is a perpetuating value upheld in the medical community, those whom do not fit in line with that value - those to whom a surprise pregnancy occurs, particularly out of wedlock - become immediate receivers of paternalistic care. Although there is extensive information to be found on - and ensuing debate on the best way to approach - teen pregnancy, information is greatly limited to preventing pregnancy, providing prenatal care, and "dealing with" a pregnant teen yet there is very little information about the experience of a teenager in the birthing space. Pregnant adolescents are unique from other groups of pregnant people in a few major ways, including social environment, personal, social, and psychological development, and physical response to pregnancy. Inadequate prenatal care (further explored later in this article) is common among teen pregnancy, with only about 65% of pregnant adolescents receiving care in their first trimester, theoretically due to financial constraints, lack of insurance, lesser access to resources, and language and cultural barriers (possibly including family and social stigma) (Tilghman). Childbirth educators offer a unique opportunity to provide support and information to pregnant adolescents in a non-clinical environment. However, the role of a childbirth educator working with teens is much different - due to the unique needs of the adolescent group - than when working with adult pregnancy. Training in challenges unique to adolescent pregnancy as well as training in the developmental needs of teens can help educators provide appropriate and useful services. Utilizing community spaces such as churches within communities (as opposed to classes held in a hospital or clinic setting) or schools can alleviate the burden of transportation that often prevents young people from accessing resources. Due to financial constraints, municipal budgeting that includes childbirth education for teens could help offset the costs of the educator and allow the pregnant people to access care more easily. Community programs such as Maternity Care Coalition offer free resources including classes and doula support to low income families and teens across the Southeastern Pennsylvania area. Knowledge of health risks unique to youth (such as greater effects of peer pressure and social status) and the physical effects of metabolic changes in the adolescent body on pregnancy (such as increased likelihood of toxemia) need to be addressed by educators. Simply creating a safe space for adolescents to talk about their experiences and have a facilitator listen can make a world of difference for everyone involved. Educators are able to gain insight into the unique challenges teens face and the participants are able to find autonomy in expressing themselves and using their voice (which is great practice for utilizing their voice in their labor process and onward in parenting and life). From Ashley, mother: A provider's experience or belief system has the potential to dictate the care they provide in labor and their support or lack thereof for the client's wishes. When a provider has been trained in a limited number of conditions (such as only in hospital birth, primarily with medicated births, in an environment with a high cesarean rate, etc.), the belief that this is representative of how birth best unfolds becomes ingrained. According to a study published in the Journal of American Medical Association, one of the main reasons providers are reluctant to provide evidence based care is because they believe what they are already doing is working. Some providers choose to ignore evidence based information simply because they believe something else works just as well or better. If some providers are this reluctant when the evidence points to a better option, imagine the reluctance when a client requests something that is outside the "normal" routine for that provider or place of birth and can't cite the research that supports it (of course, a personal preference is legitimate whether research can be cited or not and without any obligation to provide reasoning as to why). Paternalism intersects with a strong belief system to leave the client in a position where they must either actively advocate for their own preferences (or rely on a partner or support person to do so) or concede to something with which they are not comfortable. Sometimes the pressure to make certain choices is overt yet more often it is subtle. Horizontal violence is a term used to describe the abuse or violence that workers on the same level of hierarchy inflict upon each other. This reality among nurses is explored in depth in the Evidence Based Birth podcast "Why It's So Hard to Get Evidence Based Care." This term, however, is just as applicable to the way that women interact with other women. The patriarchal system in which we have all evolved from the time of the agricultural revolution 10,000 years ago, sets women against other women. Before a level of trust or intimacy is reached (if it is at all), a subconscious need to create feelings of inadequacy or "less than" in other women often prevails. (I also want to point out here that this is a learned behavior and completely open to adjustment. This is an opportunity to take a moment to reflect, to not act on impulse, and to address one's own insecurities before projecting them on someone else.) In "Women Who Hate Other Women: The Psychological Root of Snarky," Doctor of Psychology, Seth Myers, explores the idea of female criticism stemming from feelings of inadequacy in an area of life they highly value. Traumatic birth has been defined by people birthing not feeling listened to or supported in their choices by their providers and sometimes this is as simple as a nurse doubting, questioning, or negating the laboring person's choices because it differs from the standard of care they are used to providing within the setting. From Tonya, mother: The support of a birth doula, a person trained in emotionally, physically, and informationally (yet non-clinically) providing care to a pregnant and laboring person whom is not part of the laboring person's network of family and friends, can be a key component to a positive birth experience. Although a doula cannot guarantee a certain birth outcome, research has showed that the support of a doula can lead to increased spontaneous vaginal birth, shorter duration of labor, and decreased caesarean birth, instrumental vaginal birth, use of any analgesia, use of regional analgesia, low five‐minute Apgar score, and negative feelings about childbirth experiences. A 2017 Cochrane Review states, "Continuous support in labor may improve a number of outcomes for both mother and baby, and no adverse outcomes have been identified. Continuous support from a person who is present solely to provide support, is not a member of the woman’s own network, is experienced in providing labor support, and has at least a modest amount of training (such as a doula), appears beneficial." Although a doula does not advocate for someone's preferences, they can encourage their clients to advocate for themselves by asking questions and exploring alternatives. Their presence alone can help laboring people (and other non-professional support people that are present) feel confident in using their voices, utilizing positioning and comfort techniques for managing labor pains, and providing emotional encouragement and reassurance throughout the process. Doulas are available for all different price ranges and have varied levels of training and experience; they work for the client and are generally not associated with specific places of birth. PALS, a local Philadelphia based organization providing doula support, offers free and low cost doulas to expectant families who are unable to afford the higher cost of a private doula and works to provide support to new and experienced doulas. When birthing in the United States health system, the policies set by the hospital (lawyers and insurance companies) do not always match up with the recommendations of research. Research has found that a lag of ten to 20 years exists in hospital policy meeting research-based recommendations. This translates into commonplace or routine interventions that serve the majority of people in a certain setting but may not serve those whom are birthing differently. For example, intravenous (IV) fluids are routinely administered in most hospitals in the United States. IV fluids have some benefits including preventing a steep drop in blood pressure that can arise when an epidural is administered and raising amniotic fluid levels. There are also drawbacks to routine fluids including dilution of oxytocin in the blood stream (potentially slowing down labor and leading to augmentation) and fluid accumulation causing babies to be born at a higher birth weight (due to excess fluid) than they would be otherwise which can lead to what appears to be an excessive weight loss in the newborn after birth (which can then wind up affecting the support someone has in breastfeeding). In hospitals with a 90% epidural rate, the vast majority of clients will benefit from the administration of the fluids. However, for someone whom is choosing to birth without an epidural, the risks may outweigh the benefits. This sets a person up to either have to begin advocating for what they want from the time they arrive at the hospital (which engages the neocortex and can slow the labor process) or to succumb to routine procedures that have the potential to affect their labor and they way they perceive their participation in the decision making process. From Tammy Bradshaw, mother, professional photographer, owner of Tammy Bradshaw Photography: Birth place policies often limit rights to documentation of birth - recording and photographing. Although not everyone will want a visual reminder of their labor and birth experience, when a provider or birth place prohibits documentation, it takes away from a person's autonomy over their labor and birth and wind up placing authority in the hands of the provider rather than in the hands of the birthing person. A sign posted in the laboring room of a local Philadelphia hospital explicitly states: "Photography and filming during delivery is permitted only with the authorization of the mother and staff members involved in the delivery." After a few more lines of additional reminders as to who can and cannot give authorization, another line reads: "If there is concern that photos or videos have been taken without permission, security will be contacted. Security has the right to confiscate the recording device and erase any unauthorized photo or film." Photography of labor and birth can be an amazing reminder of the power of the body and the intensity of the birthing process (a recording that, of course, some people want to treasure and of which others do not want a reminder). Support people - family, friends, and doulas - may be the ones snapping pictures (with consent of the laboring person) while some people hire a professional photographer to document the experience. Because hospital policy leaves the authorization of photography up to the staff at the birth and with most birthing people utilizing a large practice of providers, it is unknown whom will be there during labor, it's common to not know how documentation will be received until someone actually comes in to the birth place ready to have their baby. Some providers are comfortable with still photography but draw the line at recording the moment of birth (or video recordings, period, in some cases). Recording on phones often leaves one unaware as to whether the documentation is still or video so many providers flat out refuse to allow pictures at the moments just before, during, and after birth. The concern here, for providers, is liability. Yet the concern for parents is that they are being forced to relinquish visual mementos from their child's entrance into the world (and the incredible expressions captured on the faces of loved ones as the baby emerges). From Rachel Utain-Evans, mother, birth photographer and videographer, owner of Rachel Utain-Evans Photography: The microcosm of the care system reflects an ability on the provider's part to override hospital policy and provide a more personalized approach to routine intervention and medical recommendations. However, research (that was focused mainly on physicians) published in the Journal of American Medical Association has shown that a provider's reluctance to provide evidence based care is due to several reasons including not being aware of the evidence, not believing the evidence, preferring the status quo, not wanting anything to change, and thinking that changes in their practice won't change anything on a larger scale (Dekker). It may seem like a stretch to suggest that care provided by clinicians is based just as much on their own personal belief as it is on research yet it is a dilemma that contributes to a lack of evidence based care in the conventional hospital setting. An example of this is the common recommendation for birthing people to push out their babies in a semi-reclined or fully reclined (lithotomy) position. The same muscles one uses to birth a baby are those used to pass bowel movements. When a bowel movement is passed, we don't commonly do it in a reclined position. In fact, it just wouldn't make much sense to us at all, based on our knowledge of gravity and the efficiency of the muscle's power when upright versus reclined. However, the high rate of epidurals in the United States (we have a national rate of 71% [Butwick]) , the lack of one on one nursing care that would allow for upright positions even with pain medication, and the greater need to intervene in second stage labor when epidurals have been administered means that the majority of people birth reclined. This means that the majority of providers whom have been trained in a hospital setting (the only setting where epidural medication is an option) - which is the majority of providers due to American Board of Obstetricians and Gynecologists training requirements - catch babies when people are reclined and feel most comfortable with clients in this position because it what they are most familiar with. This means that, even in an unmedicated birth where someone has ample ability to move into a squat or an all fours position - two positions that anthropological research show are most common when people are not told what position to birth in - they are told to birth reclined. Although our cesarean rate is twice the World Health Organization's recommended rate, we do still have the majority of people birthing their babies vaginally. Therefore, providers see this position work most of the time, which could be viewed as a true testament to the power of labor since this position typically creates less space in the pelvic outlet, does not use gravity, and compresses the descending aorta which is bringing blood to the pelvic region and the placenta (which is providing oxygen through the blood to the baby) - but providers may interpret as a position that works well. This is a prime example of two different ways of viewing the same scenario, one of which is research based and one of which is based on belief. From Anonymous: Over the past several years, there has been a shift in how labor support people are recognized and named - a shift that reflects the consciousness of changing family structure, parent autonomy, and gender, parent, and relationship identity. When a person or couple in labor encounters their provider - nurse or midwife or doctor - for the first time in labor, a common occurrence in our current care system, assumptions may be made on the part that lead to inaccurate naming of support people. There is still frequent use of the term "husband" even when that term does not apply; it is also commonly assumed in female same sex couples that the partner or wife is a sister or friend. This intersects with implicit bias to create a potentially tense dynamic between the client and the provider. An extremely easy way to ensure this does not occur is for providers to introduce themselves and ask each support person their relation to the laboring person rather than assume. The term partner can be easily adapted (and is commonly used by birth workers, especially when talking to a group of expectant parents where everyone's relationship status is different or unknown) to labor and birth situations. A doula with whom the laboring person or couple has already developed a trusting relationship can also use the appropriate term in the presence of the provider to ensure that the status is defined accurately or could even let the provider know ahead of time how the partner prefers to be named. A greater awareness and the use of appropriate terminology allows the provider to begin formulating a positive relationship with the laboring person and support people from the beginning which allows for the creation of a less stressful environment. Transgender and gender non-conforming people are another incredibly marginalized group of birthing people. People who are transgender identify with a gender other than the sex they were assigned at birth. The number of transgendered adults in the United States is estimated to be about 1.4 million (Estimate of U.S. Transgender Population). Non-binary people relate to their gender in a way that falls outside of the gender binary (the "gender binary" meaning to have two parts - male and female - and non-binary meaning to not fall into either of those categories some, or all of the time) and have been recognized by cultures worldwide for millenia (Understanding). People describe their trans identities in many different ways, including but not limited to assigned female at birth, assigned male at birth, female to male, male to female, trans man, trans woman, gender non-conforming, agender, genderfluid, and genderqueer.* Efforts to maximize health, safety, and respect in the current care system need to include language, education, and research that is specifically applicable to every group of birthing people and the understanding of what applies to whom must be incorporated. To date, despite the greater visibility of people identifying as transgendered and non-binary whom are birthing babies, little research exists that looks solely at the reproductive needs of transgender men in pregnancy (and the few studies we do have are done on white middle class people which excludes a significant population). The lack of research is a glaring sign that, in both midwifery and obstetrical culture as well as childbirth education and reproductive justice, we have a long way to go and a steep hill to climb in order to provide competent care. A small study published in BMC Pregnancy and Childbirth concluded that improving clinical visibility and affirming gender has the potential to not only lead to increased client satisfaction in the care received during the childbearing year but also may support client centered perinatal care services, as lack of understanding of gender identity from health care providers is a leading barrier for transgendered people receiving health care services. Providers can make changes in their practices to offer trans inclusive care including the use of inclusive language, changing of intake forms that ask questions based largely on gender, and requiring trans competency training for all staff. It is also incredibly important for providers to maintain transparency about their experience and knowledge of trans care and ask direct and respectful questions, only of which are relevant to the care they are providing (Rachlin). From Philadelphia birth worker Jenna Brown, owner of Love Over Fear Wellness and Birth: Cultural biases and language conventions are driving forces in the way in which we view, name, and discuss aspects of childbirth and those whom are involved and therefore are inseparable from the care people experience. Although implicit bias is not necessarily intentional, this does not change the impact of that bias. When education and training is steeped in a Eurocentric perspective rather than evidence-based information, the disconnect between provider and patient becomes glaring. A language barrier or the use of medical jargon - its own form of language barrier - creates a divide between provider and patient and the birthing person immediately loses power when discomfort is felt or lack of understanding occurs (increasing anxiety and stress). When the language of birth is saturated in "woman" and "mother" and "she," with no adjustment for the gender identity of the person giving birth, the person laboring loses autonomy. Terminology including "delivery" and "geriatric pregnancy" and failure to progress" only work to assert a power differential between the person in a place of medical authority and the person working through the labor process. (And just for the record, only you deliver your baby; providers catch or help to facilitate birth.) We are in an interesting space in time right now as there is a greater awareness of the ways that people identify and general encouragement to respect people's gender and relationship identity. However, there is a pushback against this inclusion that is furthered by some facets of the midwifery, childbirth education, and doula community. Organizations that certify birth workers yet refuse to change their language - or even simply add language - to their training sessions and manuals enforce a profound disrespect for those whom are birthing that don't identify as women and/or mothers and also risk alienating those whom do identify as women and/or mothers yet embrace the need to include all birthing people. The language used in trainings offers an opportunity to educate new birth workers in an inclusive approach to working with clients that can then be tailored to the needs of the individual with whom they are supporting. When organizations refuse to use inclusive language, it is a direct refusal to stand by all those whom are birthing and a dissonance is formed that only serves to propel fair, just, and informed care for some but not all. The refusal of many organizations to include language and appropriate care for those whom do not identify as women and/or mothers has been a catalyst for those whom are embracing reproductive justice for all. "Birth for Every Body" is an online resource for gender and birth and is geared for both patients and providers and includes some trainings that can be used for CEUs. This website was created by midwives in response to midwifery organizations refusal to acknowledge trans inclusive language and training. The online presence of such an easy to access and easy to navigate resource that presents information to both expectant people and professionals offers an opportunity to both find inclusive care providers and find resources in inclusive care training. There are also many birth workers whom are offering trainings to clinical and non-clinical birth professionals (and other businesses as well!) on gender inclusive practices in the workplace, in client/provider relationships, and in registration and intake forms. A few people local to Philadelphia that are offering LGBTQIA community education include Ray Rachlin, LM, CPM, CLC and Jenna Brown, birth doula. The argument for resistance to use birthing terms appropriate for all (or even incorporating those words into the common birthing language) is often that it feels like an attempt to erase "woman" from birth. It is understandable to the extent that "women" have, and continue to be, viewed as a second class group of people in the social structure (one only needs to look at pay disparity, balance of work inside and outside the home, and the horizontal violence between one another to begin to see the social impact of this) and to own and claim the world of birthing as that of the woman allows ownership of something that no one can "take away." However, the reality is that people who do not identify as woman do also give birth so to deny that is just simply unrealistic (and far more complex as well). If someone lives their life as a man or as a non-binary person, refers to themself as a man or non-binary person, and chooses to use their internal organs to carry and birth a child, why should that person be referred to as anyone other than whom they identify? If someone is concerned about the "womanly" world of birth being taken away from them, one need look no further than the fall of midwifery and rise of obstetrics in American history (in which a long cultural history of midwifery - both within communities of color relying on "granny midwives" and communities relying on European midwives was annihilated by an overwhelmingly patriarchal system of medicalization of childbirth). Those running group trainings or sessions can ask for the pronouns of those attending, can use language to reflect and include all birthing people yet can also, when appropriate in situations where the gender identification of people is known, be more specific. The eradication of "woman" and "mother" from pregnancy and birth is not at stake here; it is simply being expanded so that all birthing people get the respect all people deserve. From Jodi Silberstein, Doula: Access to prenatal care is often limited by factors including financial and economic status, transportation, childcare, work, language, fear of deportation, teen pregnancy, drug use, and displeasure at the pregnancy. Hospitals are not legally allowed to turn away people in labor that come through their doors. However, private practices can refuse prenatal care to those without insurance, whom are unable to pay, or whose insurance will not cover certain services. This limits access to prenatal care and prenatal testing simply based on income and economic status. When people know they will not be able to get services, they are less likely to attempt to find a willing provider. When they try to obtain services, providers are extremely limited, if existent at all, since payment is not guaranteed. Medicaid does cover perinatal care for pregnant people but the time spent waiting for eligibility to be determined and coverage to kick in leaves many people without access to care for a significant portion of their pregnancy. However, according to Dr. Robert Ferrer, a family physician interviewed in the article "Behind From the Start," the easiest way to quickly obtain care is to have a primary provider that one can call as soon as they realize they are pregnant. Unfortunately, those without insurance are less likely to have a healthcare provider they can call; this leaves people feeling unsure as to the first steps in obtaining prenatal care. The need to travel to appointments and possibly wait for hours to see a provider means that people means having to arrange and pay for transportation, possibly bringing other children with them or paying for childcare, and, on top of it all, possibly losing wages due to missing work - all discouraging of accessing prenatal care. Immigrants often fear that deportation will result from utilizing the healthcare system and therefore do not attempt to find care. According to date from the 2016 national birth file looking at 100% of births registered in all 50 states and the District of Columbia, 15% of people giving birth received inadequate care during their pregnancy (CDC). Interestingly, a 1995 review of the effect of prenatal care on birth outcomes has shown that, aside from the potential complications of low birth weight which can be correlated to lack of prenatal care, prenatal care has little effect (Fiscella). This may point to the faults of the reproductive care system as a whole in providing adequate care to improve outcomes. Whether adequate prenatal care specifically improves outcomes depends on the factors being assessed under the heading of "outcomes." Outcome could be assessed as physical health of the birthing person, physical health of the baby, emotional well-being in the postpartum, satisfaction with birth outcome, feelings of support during the perinatal period, access to additional community resources, and more. The review mentioned above cites the limitations in assessing only the most basic definition of "outcome" - maternal and infant morbidity and mortality. In the documentary "Why Not Home?," it is suggested that free access to prenatal care - such as the care provided at The Easy Access Clinic, founded by CPM Jennie Joseph - may improve birth outcomes because it may increase interest in midwifery care and out of hospital birth. The Easy Access Clinic, located in Central Florida, is based on the belief that everyone deserves access to quality medical care. They accept insurance (including Medicaid), they offer sliding scale payment, and they don't turn anyone away for lack of ability to pay. The clinic has had amazing statistics for demographics commonly marginalized in the larger reproductive health system. The adherence to principles including but not limited to freedom of choice, easy access, self reliance, and education, part of an approach Joseph has created called "The JJ Way", have improved birth outcomes, while the personalized social support that can come from care without any fear attached helps to create positive pregnancy and birth experiences. The outcome of providers and organizations coming together in hopes of addressing and remedying this disparity in access to prenatal care has the ability to address the continuum of support for families that is a break in the full spectrum of adequate health care. It is also well documented by the World Health Organization that increased access to midwives can lead to better reproductive care and better health outcomes for both the parent and baby. Among other statistics, WHO states that "56 maternal and neonatal outcomes were found to be improved through midwifery practice and philosophy of care" (World Health Organization). Midwifery care can be provided in a hospital, birth center, or home setting and it is estimated that midwives could safely provide care for about 80% of reproductive health care needs when trained to universal standards (such as those advocated for by the International Confederation of Midwives). This model of care is cost effective and safe and associated with reduced maternal and neonatal morbidity, reduced interventions in labour, improved psycho-social outcomes, and increased birth spacing and contraceptive use (Sandall). Less than 10% of births in the United States are attended by midwives and just slightly more than 1% take place outside of a hospital (according to statistics from 2013, 64.4% of the 1.4% of out of hospital births took place at home and 30.2% of the 1.4% took place in a freestanding birth center) (CDC). There are only about 350 freestanding birth centers nation wide (with two available right here in the greater Philadelphia area!). Greater government support of midwifery care could increase the availability of birth centers and therefore increase access to midwifery based care. Despite a study of over 16,000 people that showed planned homebirth to be as safe as planned hospital birth (Cheyney), the lack of financial coverage by insurance makes homebirth out of reach for many people. It is easier for someone to pay a $1000 deductible for a $13,000 uncomplicated vaginal birth in a hospital than it is for someone to pay $4000 to $7000 out of pocket for an uncomplicated homebirth. Although midwives are covered by Medicaid under the Affordable Care Act, private insurers may not cover midwifery care. Greater insurance coverage may lead to greater access to midwifery care, which is an important component of reducing morbidity and mortality, reducing health care costs, and providing more supportive care for normal birth. The disjointed care system - the lack of collaboration between obstetricans and midwives - leave many birthing people having to choose between one or the other. Birth centers have the support of a back-up hospital but often give up a significant amount of autonomy when the transfer of care to a hospital takes place. Clients become subject to the policies of this new birthing place and the birth center provider has very little leeway when it comes to individualized care in that setting. If a low risk pregnant person chooses to birth at home under the care of a skilled midwife and it is decided in labor that a transfer to the hospital is safest, many people transfer to the closest hospital. When the midwife has not been integrated into the larger system of care, the transfer can be quite stressful. "If midwives were allowed to work alongside other providers, patients would get the care advantages, and if difficulties arose, a woman whose home birth suddenly became complicated could be seamlessly transferred to a hospital" (Editors) A study that looked at the integration of midwifery care from state to state in the U.S. found that states that ranked best (defined by having fewer preterm births, underweight newborns, and cesarean birth) had licensing requirements for different types of midwives, gave midwives the ability to care for people in different settings, write prescriptions, and receive payments from Medicaid (Vedam). In an article published by Reuters, lead study author Saraswathi Vedam stated, "The question is not whether it is better to have a midwife or a doctor, but the degree to which midwives and doctors are able to work together to provide the best care utilizing all of their expertise and abilities." This perspective reflects one of the Common Ground Statements from the The Home Birth Summit Collaboration Task Force, a group of national reproductive care leaders including physicians, midwives, researchers, health administrators, payors, policymakers, and consumers that have come together to improve maternity care in the U.S. in all settings. The Common Ground Statement reads: "We believe that collaboration within an integrated maternity care system is essential for optimal mother-baby outcomes. All women and families planning a home or birth center birth have a right to respectful, safe, and seamless consultation, referral, transport and transfer of care when necessary. When ongoing inter-professional dialogue and cooperation occur, everyone benefits." From Anonymous: Increased access to health insurance, high quality care, and providers that practice patient-centered and culturally sensitive care has the potential to decrease maternal and newborn mortality and morbidity and also paves the way for an emotionally secure experience that can be easier integrated into the postpartum period. Although the homebirth setting is not for everyone - whether that be for medical or personal reasons - the model of care exhibited by homebirth midwifery has the potential to bring individualization back into the birthing process. Homebirth midwives tend to develop a fairly intimate relationship with their clients, often recognizing them when seeing them out in public years after catching their babies. To a homebirth provider, the client is a face and a name and a story and the care provided to each person varies slightly depending on this holistic view. Prenatal care is provided by the midwife in addition to continuous care throughout the labor process (without shift changes). This is followed up by frequent postpartum support - hours spent with the family after the birth, visits on day two, day three, and then at least one more time before the six week check-in appointment. Clients will often continue to use the midwife's support through phone and text for several weeks (or months!) after birth. Because of the trusting relationship that develops with such intimate care, it is possible that fewer stress hormones are released, greater confidence in parenting is established, and the postpartum period becomes less daunting to the new family. Given the incredibly thorough care being provided by an individual midwife (and possibly their assistant), midwives are limited in the number of families with whom they can work. To extrapolate this model on a larger scale, would absolutely lead to some challenges, such as a need for a much larger number of providers to create a lesser work load for each. However, this could lead to a decrease in cesarean birth, a decrease in healthcare costs, and an easier time transitioning into the postpartum period for new families. Of course, this model of care would require an entire overload of the system - possible but challenging to accomplish. From homebirth midwife Christy Santoro, CPM: Postpartum support, although not often the focus of reproductive health, is a realm almost untouched by the current care system. For those birthing in a hospital, postpartum follow up after leaving their birth place is limited to a six week follow up visit. This leaves SIX WEEKS with a new baby, a body leaking fluid, blood, and milk, a hormonal roller coaster, and possibly limited help from family and friends before a check in occurs with a health care professional. Thankfully insurance companies often offer free home visits with a nurse and lactation consultant that clients can take advantage of in the weeks between coming home and seeing their provider. However, many people do not realize this is even available, some meetings are limited to the visiting nurse's availability within a specific time frame, and, again, new parents find themselves meeting with a new care provider with whom they lack the trust and intimacy that comes with prior meetings. With perinatal mood disorders, including depression, anxiety, and obsessive behavior, arising anywhere within the first year after giving birth and affecting 15 to 20% of the population, the support a new family receives can quite literally make or break the weeks and months after giving birth. Research from late 20th and early 21st centuries suggests that postnatal depression is more prone in Western culture due to increased isolation and less traditional gender roles. However, a study from the year 2000 analyzed the postnatal depression symptoms of 900 women from five continents and found that depressive symptoms were greater in non-Westernized countries (Affonso). The question, then, becomes how can we best support new families in having their individual needs met, their parenting style affirmed, their cultural traditions explored in a way that leaves opportunity for adjustment and flexibility, and building and utilizing community resources? From mother, Alison: The support of a postpartum doula can be a critical factor in the transition into a healthy family dynamic. Postpartum doulas offer hourly help to the new family so that they can spend time bonding, establishing feeding, resting, and getting to know their baby. The doula comes with knowledge of childbirth, maternal postpartum health, infant care, and feeding yet is also equipped and prepared to make meals, run errands, walk pets, and lightly clean the house. Since postpartum doula support is not covered by government in the U.S. as it is in some other states, families must pay out of pocket for this type of support (rates range from $25 to $35 an hour generally). At a time where income is often decreased by the birth parent taking leave, it can seem like quite a stretch for parents to procure the support of a postpartum doula. Prioritizing this support, however, may mean that family and friends could chip in to cover the cost or offer it as a baby shower or postpartum gift. Prenatal infant care and postpartum wellness classes offer parents an opportunity to explore the realities of life with a newborn and prepare in advance for the support they may need. Classes often cover the myths and realities of expectations of newborn behavior, feeding patterns, and sleep in the first six weeks or so after birth and go over the basics of caring for a baby. Postpartum wellness classes include information about the hormonal ups and downs of the postpartum period, the physical and emotional needs of both new parents, and tips for easing the transition into a new family dynamic. These classes are often offered by childbirth educators and/or doulas and may be part of a childbirth class series or an additional class option. The importance of birth is not only in the birth itself but is truly in the understanding that labor is the starting point for a much larger transformational journey. When that journey begins and proceeds in a positive and supported and informed way, it's like beginning a long trek through uncharted territory with an up to date map and a lot of knowledge of the flora and fauna, and echo of the words of wisdom from those whom have successfully made their own treks before. In contrast, when that journey begins in fear and anxiety and with little information, it's the equivalent of beginning a trek after a night without sleep, when your map has spilled coffee on it, and you don't know a single person whom has ever journeyed in this way before, all the while you have a nagging feeling that some sort of animal is tracking you but you can't quite place it's location. When the supporters of birth and the transformation of parenting have the opportunity to provide solace, to build confidence, to encourage someone to claim their autonomy in their journey, it is that support person's innate responsibility to embrace that opportunity. The need to constantly reevaluate oneself and one's practice for the greater good can only arise when we break free of the conventions that hold us down and face the uncertainty of giving ourselves to one another without greater agenda. In offering that, we rise up together and make change. *Thank you to Jenna Brown, doula and founder of Love Over Fear Wellness and Birth, for their guidance and editing assistance.* SOURCES CITED
Affonso, DD. et al. An international study exploring levels of postpartum depressive symptomatology. Journal of Pscyhosomatic Research, 2000 Sep;49(3):207-16. Alexis Hoffkling, et al. “From Erasure to Opportunity: a Qualitative Study of the Experiences of Transgender Men around Pregnancy and Recommendations for Providers.” BMC Pregnancy and Childbirth, BioMed Central, 8 Nov. 2017. Belasco, Jessica Claire. “Behind from the Start: Why Some Women Aren't Receiving Early Prenatal Care - Part 2.” Center for Health Journalism, www.centerforhealthjournalism.org/fellowships/projects/behind-start-why-some-women-arent-receiving-early-prenatal-care. Cheyney, Melissa, et al. “Outcomes of Care for 16,924 Planned Home Births in the United States: The Midwives Alliance of North America Statistics Project, 2004 to 2009.” Journal of Midwifery & Womens Health, vol. 59, no. 1, 2014, pp. 17–27., doi:10.1111/jmwh.12172. Butwick, Alexander J., et al. “Maternal Body Mass Index and Use of Labor Neuraxial Analgesia:A Population-Based Retrospective Cohort Study.” Anesthesiology, The American Society of Anesthesiologists, 1 Sept. 2018. CDC. "National Vital Statistics Report." 2015. PDF file. Chalhoub, Theresa, and Kelly Rimar. “The Health Care System and Racial Disparities in Maternal Mortality.” Center for American Progress, www.americanprogress.org/issues/women/reports/2018/05/10/450577/health-care-system-racial-disparities-maternal-mortality/. Culp-Ressler, Tara. “The Myth Of The Absent Black Father.” ThinkProgress, 26 January 2014. Culturedcreative. “Growing Stigma around Unmarried Motherhood.” Mother and Baby Homes, 26 July 2013, motherandbabyhomes.wordpress.com/2013/07/26/growing-stigma-around-unmarried-motherhood/. Declercq, Eugene R. et al. Childbirth Connection. “Listening to Mothers III: Pregnancy and Birth. Report of the Third National U.S. Survey of Women’s Childbearing Experiences.” May 2013. http://transform.childbirthconnection.org/wp-content/uploads/2013/06/LTM-III_Pregnancy-and-Birth.pdf. Dekker, Rebecca. “Evidence on: IV Fluids During Labor.” Evidence Based Birth. 24 May 2012; updated 31 May 2017, https://evidencebasedbirth.com/iv-fluids-during-labor/. Dekker, Rebecca, narrator. "Why it's so hard to get evidence based care." Evidence Based Birth, ITunes app, Episode 3. DONA International. Benefits of a Doula, 10 Apr 2019. https://www.dona.org/what-is-a-doula/benefits-of-a-doula/. “Easy Access Clinic.” Easy Access Clinic, easyaccessclinic.com/. Editors. "The U.S. Needs More Midwives for Better Maternity Care." Scientific American, 1 February 2019. “Education and Training for OB/GYN.” Chicago Medicine, chicago.medicine.uic.edu/departments/academic-departments/obstetrics-and-gynecology/education/medical-student-education/obgyn-student-interest-group/education-and-training-for-obgyn/. Elmir, R. et. al. Women’s Perceptions and experiences of a traumatic birth: a meta-ethnography. Journal of Advanced Nursing, 2010 Oct; 66(10):2142-53. "Estimate of U.S. Transgender Population Doubles to 1.4 Million Adults." The New York Times, 30 Jan 2018. https://www.nytimes.com/2016/07/01/health/transgender-population.html Fiscella, K. “Does Prenatal Care Improve Birth Outcomes? A Critical Review.” Obstetrics and Gynecology, Centre for Reviews and Dissemination (UK), Mar. 1995, www.ncbi.nlm.nih.gov/pubmed/7862395. Headley, Megan. “Could Legally Mandated Racial Bias Training Reduce Maternal Mortality Rates for Black Women?” Patient Safety & Quality Healthcare, www.psqh.com/analysis/could-legally-mandated-racial-bias-training-reduce-maternal-mortality-rates-for-black-women-2/. Home Birth Summit. Common Ground Statements from The Home Birth Summit Collaboration Task Force. www.homebirthsummit.org. Italiano, Laura. "More babies are being born to unmarried parents in U.S. than ever." New York Post, https://nypost.com/2018/10/17/more-babies-are-being-born-to-unmarried-parents-in-us-than-ever/. Leavy, Patricia, and Patricia Leavy. “Single-Parent Families Are Not 'Less Than' Two-Parent Families.” HuffPost, HuffPost, 10 Oct. 2017, www.huffpost.com/entry/a-conversation-about-single-parenting_n_8981898. Livingston, Gretchen, and Gretchen Livingston. “The Rise of Single Fathers.” Pew Research Center's Social & Demographic Trends Project, Pew Research Center's Social & Demographic Trends Project, 24 Sept. 2013 “Lost Mothers: Maternal Mortality In The U.S.” NPR, NPR, www.npr.org/series/543928389/lost-mothers. Mathur, Aparna, and Hao Fu. “The Mysterious and Alarming Rise of Single Parenthood in America.” The Atlantic, Atlantic Media Company, 13 July 2015. McCollum, Brittany Sharpe. "Every Laboring Person's Rights." Modified from "Rights of Childbearing Women," Childbirth Connection, www.childbirthconnection.org/rights. Moore, Jessicca. Why Not Home?, 2016. “Neel Shah, MD, MPP.” Home, scholar.harvard.edu/shah/home. Office of Adolescent Health. “Trends in Teen Pregnancy and Childbearing.” HHS.gov, US Department of Health and Human Services, 25 Apr. 2019, www.hhs.gov/ash/oah/adolescent-development/reproductive-health-and-teen-pregnancy/teen-pregnancy-and-childbearing/trends/index.html. Osterman, M.J.K. and Joyce A. Martin, M.P.H. "Timing and Adequacy of Prenatal Care in the United States." National Vital Statistics, May 2018. “Paternalism | Definition of Paternalism in English by Oxford Dictionaries.” Oxford Dictionaries | English, Oxford Dictionaries, en.oxforddictionaries.com/definition/paternalism. Perez, Zoila Miriam. Interview by Dr. Kenya Beard. "Race and Maternal Death Rates - Black Women and Babies bear the greatest risk." Web. “Pregnancy & Postpartum Mental Health Overview.” Postpartum Support - PSI, www.postpartum.net/learn-more/pregnancy-postpartum-mental-health/. Rachlin, R. (Producer). (2019). Making Your Birth Work Trans Inclusive [Video webinar]. Roozbeh, Nasibeh, et al. “Barriers Related to Prenatal Care Utilization among Women.” Saudi Medical Journal, vol. 37, no. 12, 2016, pp. 1319–1327., doi:10.15537/smj.2016.12.15505. Sandall J, Soltani H, Gates S, Shennan A, Devane D. "Midwife-led continuity models versus other models of care for childbearing women". Cochrane Database of Systematic Reviews, 2016, Issue 4. Simkin, P. “Birth Trauma: Definition and Statistics.” PATTCh, pattch.org/resource-guide/traumatic-births-and-ptsd-definition-and-statistics/. Simkin, P. Just another day in a woman's life? Women's long-term perceptions of their first birth experience. Part I. Birth, 1991 Dec; 18(4):203-10. Sistah of the Yam, L.L.C. Expecting Possibility. 2019. “Single Mom Statistics: Surprising Facts & Figures Of Today's Single Mother.” Emma Johnson, 12 Mar. 2019, www.wealthysinglemommy.com/single-mom-statistics/#ref12. "'So you're crazy?': the cultural barriers that make postnatal depression worse." The Guardian. https://www.theguardian.com/australia-news/2018/apr/28/so-youre-crazy-the-cultural-barriers-that-make-postnatal-depression-worse Tilghman, Joan, PhD, WHNP-BC and Avi Lovette, MSN, FNP-C. "Prenatal Care: The Adolescent's Perspective." Journal of Perinatal Education, 2008 Spring; 17(2): 50–53. “Understanding Non-Binary People: How to Be Respectful and Supportive.” National Center for Transgender Equality, 5 Oct. 2018, transequality.org/issues/resources/understanding-non-binary-people-how-to-be-respectful-and-supportive. Vedam, Saraswathi, et al. “Mapping Integration of Midwives across the United States: Impact on Access, Equity, and Outcomes.” PLOS ONE, Public Library of Science, journals.plos.org/plosone/article?id=10.1371/journal.pone.0192523. Villarosa, Linda. “Why America's Black Mothers and Babies Are in a Life-or-Death Crisis.” The New York Times, The New York Times, 11 Apr. 2018. “Women Who Hate Other Women: The Psychological Root of Snarky.” Psychology Today, Sussex Publishers, www.psychologytoday.com/us/blog/insight-is-2020/201309/women-who-hate-other-women-the-psychological-root-snarky. World Health Organization. The Case for Midwifery, 1 May 2018, https://www.who.int/maternal_child_adolescent/topics/quality-of-care/midwifery/case-for-midwifery/en/. 16 Apr 2019. Anxiety can be such a large and unwelcomed part of life. Pregnancy can bring on additional stress that exaggerates feelings already present or never before felt. It's an honor to have psychotherapist Katie Wenger share on this important topic. - Britt  Pregnancy is probably one of the most vulnerable times during our lives. When you are preparing to welcome a new baby into the world, your family, and your life, there are a lot of thoughts and emotions that surface. Sometimes there are situations that cause anxiety or an increase in anxiety during pregnancy that may be health or family-related. Other times, anxiety may be occur unexpectedly. If we really look into this anxiety, particularly the anxiety that can’t be linked to a particular stressor, there is a lot that can be learned about yourself and how you process your emotions and information. You can gently explore what lies beneath specific worries or general anxiety. You can then identify what can be released and what must be addressed. The thoughts that can be released can be worded into a type of mantra or phrase that you can repeat to reassure yourself and change your mindset. There is relief in support. The support of a pregnancy or birth team, family, a partner, or friends can facilitate the expression of these emotions and the reassurance that you are not alone. It is very important to communicate any concern that you have about managing your anxiety or emotions to a trusted person that can connect you to the right resources. This may be a therapist or someone else with whom you feel comfortable being in this role. Therapy can also be extremely helpful during this time to express your emotions out loud and assess what strategies are the most helpful to you. Meditation can help you relax your body, de-stress, and connect with your baby. Here is one that I like from the app, Insight Timer: Institute of Noetic Sciences - Grounding Meditation for Pregnant Women & New Moms I found pregnancy meditation so comforting and relaxing during my own recent pregnancy. And even though your little one is still snugly secured inside of you, it also sets the stage for teaching your children meditation and allowing them to feel the calming and reassuring effects of meditation and deep breathing. And we know that relaxing and taking in deep cleansing breaths benefits our babies! Nutrition and exercise are always so important in taking care of yourself and are especially important when trying to decrease your anxiety during pregnancy. Light exercise can go a long way including a nice calm walk. Assessing and talking with a nutrition or health-care professional about your nutritional needs and how to best meet these needs can be very helpful. And most of all, go easy on yourself as you notice and work through any anxiety during pregnancy. Don’t judge what you’re feeling or your reactions and release any shame or stigma. Be compassionate towards yourself - you are the most important person to play this role for you.  Katie Wenger LCSW is a psychotherapist based in North Wales, PA but also travels to homes in the Philadelphia suburbs for sessions. She specializes in anxiety and how anxiety affects relationships. After 14 years as a therapist, the most effective approach has emerged. She believes in having a clear plan for sessions and continuing to find and utilize creative techniques and recommendations. Outside of the office, Katie spends her time doing yoga, running, reading, and raising her blended family. You can find her at katiewengerlcsw.com or reach out directly by e-mailing [email protected] or by phone at 267-304-4442.  It's back to school already. Somehow it really snuck up on me this year. So what could make the hectic mornings and whirlwind after-school pre-dinner window just a bit easier to manage? ABC muffins of course! I've adapted these from a parsnip spice cake recipe a client shared with me years ago. They are nutrient dense, free of refined sugars, free of animal products, full of flavor, AND are moist as can be. Trust me - they are amazing! I like to make a double batch and freeze some for later. ABC Muffins (apples, bananas, carrots) 3 to 4 mashed bananas 1/4 cup coconut oil 3tbsp blackstrap molasses 1 tsp baking soda 1/2 tsp salt 1 tsp ground ginger or 1 tbsp fresh grated ginger pinch of cloves 2 tsp cinnamon (you can lessen this if that's over the top for you) 2 cups very coarsely grated carrots 1 cup whole wheat flour 2 medium apples finely diced **pre-shredded carrots are a huge time saver!** Preheat the oven the 350. Grease a 12-cup muffin tins (or line with cupcake papers). In a medium bowl, whisk together the bananas, oil, molasses, baking soda, salt, ginger and cloves. Add the carrots and whisk thoroughly. Stir in the flour, add the apples, and mix until thoroughly combined. Fill the muffin tins three-quarters full. Bake until a toothpick inserted into the center comes out clean, about 30 minutes. Let cool for 5 minutes in the pan before inverting onto a cooling rack to cool completely. Enjoy! |
AuthorAs the Philadelphia birth world blooms bigger and brighter, I think it's time I start putting some of the insightful questions I've received and information I've research into a public journal. I hope you'll find this inspiring, empowering, and totally enjoyable. Archives
February 2021
Categories |

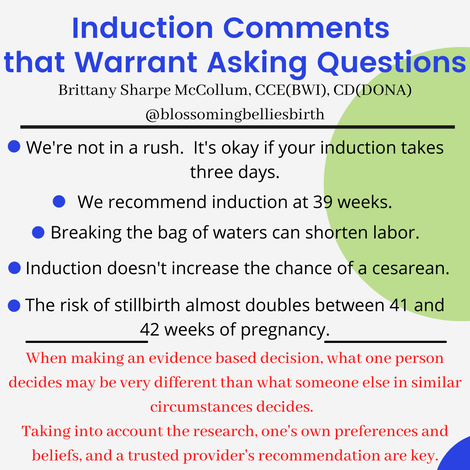
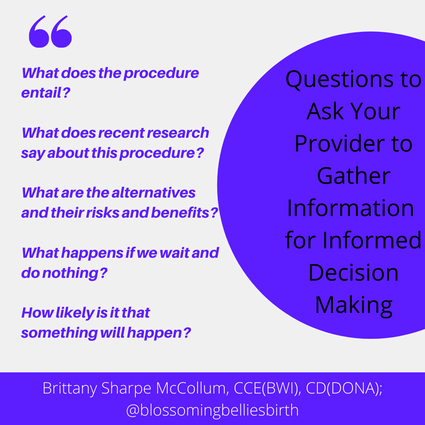


 RSS Feed
RSS Feed